Weight control and diet - InDepth
Obesity - managing your weight - InDepth; Overweight - managing your weight - InDepth; Healthy diet - managing your weight - InDepth; Weight loss - managing your weight - InDepth; Dieting - InDepth; Obesity - InDepth; Weight loss - InDepthAn in-depth report on losing and managing weight safely for health benefits.
Highlights
Overview
- A stable weight depends on a balance between the energy you get from food and the energy you use.
- When a person consumes more calories than the energy they use, the body stores the extra calories in fat cells (adipocytes or lipocytes).
- When a person uses more calories than they consume, they will lose weight.
Obesity Epidemic in Children
- Today 18% of children (ages 6 to 11) and 21% of adolescents (ages 12 to 19) in the United States are obese. The prevalence of obesity in American children and adolescents has risen dramatically over the past two decades and continues to increase.
- Children who are obese need to be screened regularly for the same comorbidities as overweight adults, including hypertension and diabetes.
- Teaching parents healthy lifestyle skills can lead to a sustained weight reduction in moderately obese children, including those in ethnically diverse populations.
- School-based physical activity programs do not seem to promote greater overall activity levels or weight loss in children. Parents should not depend on schools to motivate good diet and exercise habits in their children.
Obesity in Adults
- Adult body mass index (BMI) is considered normal between 18.5 and 24.9 kg per square meter (kg/m2) and above; this article will use these units unless otherwise stated. A BMI of 25 to 29.9 is in the overweight category. Obesity is a BMI of 30 and above.
- According to the latest figures available (2015-2016), 39.8% of American adults (age 20 and older) are obese, and 71.6% are obese or overweight.
- Worldwide around 39% of all adults ages 18 and above are overweight, and 13% are obese.
- Being obese, particularly with a BMI over 35, is associated with a significantly higher death rate.
- Weight loss in obese individuals significantly lowers the risk of health problems and early death. For example, knee pain may be significantly reduced with weight loss through a diet and exercise program.
Lifestyle changes
- Lifestyle changes, including diet and physical activity, can be used alone or in combination with medications, psychotherapy, or surgery for the management of obesity.
Medication
- Obesity medications are typically used in combination with lifestyle changes.
- Liraglutide (Saxenda) is approved as the fifth available obesity drug in the United States. It is approved for use when a medical problem such as high blood pressure, diabetes, or elevated cholesterol is also present. Liraglutide is used to help control blood glucose in type-2 diabetics, but may promote weight loss in some patients. This medication is given by injection.
- Other drugs available include phentermine/topiramate (Qsymia), lorcaserin (Belviq), bupropion/naltrexone (Contrave), and orlistat (Xenical).
- Obesity medications have been shown to help reduce risk factors for heart disease, but they have not yet been proven to reduce the risk of cardiovascular events or death, except in people with type 2 diabetes.
Surgery
- Patients who have bariatric surgery lose more body weight compared to patients receiving nonsurgical treatment.
- Studies have shown that bariatric surgery appears to produce better glucose control than medical therapy alone in the short term. More research is necessary to assess long-term outcomes. Whether surgery should be recommended for patients with a BMI of 35 or greater or with a BMI of 30 or greater and comorbidities is not fully established or agreed-upon.
- Bariatric surgery does not appear better than conventional weight loss therapy for improving sleep apnea symptoms or high blood pressure.
Introduction
A stable weight depends on a balance between the energy you get from food and the energy you use. You use energy during the day in three ways:
- Energy expended during rest to maintain vital functions (basal metabolism)
- Energy used for all non-exercise activities and to break down food (thermogenesis)
- Energy used during physical activity
Basal metabolism accounts for about two-thirds of spent energy. Your body generally uses this energy to keep your temperature steady and the muscles of your heart and intestines working. Thermogenesis accounts for about 10% of spent energy.
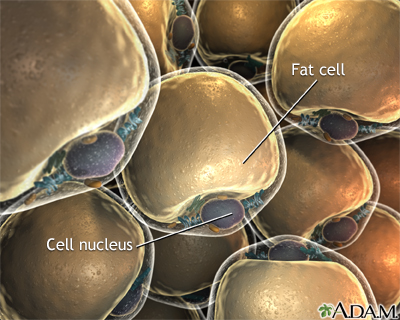
When a person consumes more calories than the energy they use, the body stores the extra calories in fat cells (adipocytes). Fat cells function as energy reservoirs. They grow or shrink depending on how people use energy. If people do not balance energy input and output by eating right and exercising, fat can build up. This leads to weight gain.
When energy input is equal to energy output, there is no expansion of fat cells (adipocytes) to accommodate excess. When you take in more calories than you use, the extra fat is stored in your adipocytes and you begin to accumulate fat.
Measurement of Obesity in Adults
Obesity is determined by measuring body fat, not just body weight. People who are very muscular with low body fat may not be obese, even if their weight is over the limit for their height. Others might be at a normal weight or even underweight, but still have excessive body fat. The following measurements and factors are used to determine whether a person is overweight to a degree that threatens their health:
- Body mass index (BMI). A measure of body fat based on weight and height, expressed as kilograms (kg) per square meter (m2)
- Waist circumference (size around the waist)
- Waist-hip ratio
- Skin fold measurement (anthropometry)
- Dual-energy x-ray absorptiometry (DXA)
A person's disease risk factors and BMI are important components in determining the health risks of their weight.
Body Mass Index (BMI)The current standard measurement for obesity is body mass index (BMI). In children, BMI is expressed as a percentile relative to the BMI of other children of the same sex and age. In adults over age 20, BMI is considered normal between 18.5 and 24.9. A BMI of 25 to 29.9 is in the overweight category. Obesity is a BMI of 30 and above. A BMI of 40 or more is considered morbidly obese and usually means men are at least 100 pounds (45 kilograms) over their ideal weight and women are at least 80 pounds (36 kilograms) over their ideal weight.
Obesity is then classified into three categories:
- Class 1: BMI of 30 to 34.9 (low-risk obesity)
- Class II: BMI 35 to 39.9 (moderate-risk obesity)
- Class III: BMI of 40 or greater (high-risk obesity)
These criteria may be used to estimate the risk for complications of obesity, such as type 2 diabetes, heart disease, obstructive sleep apnea, or certain cancers. They are also used to help decide when surgery may be most appropriate.
Calculating Body Mass IndexYou can calculate your BMI by dividing your weight in kilograms by your squared height in meters. (BMI calculators are available online.)
For example, a woman who is 5'6" (1.68 m) and weighs 130 pounds (59 kilograms) has a healthy BMI of 21. A woman at the same height who weighs 190 pounds (86 kilograms) will have a BMI of 30.7, corresponding to class 1 obesity.
You can check your BMI with the Centers for Disease Control and Prevention website -- BMI calculator.
Waist CircumferenceWaist measurement is another way to estimate how much body fat a person has. Extra weight around the midsection or stomach area increases the risk for type 2 diabetes, heart disease, and stroke.
Some studies suggest that:
- Women whose waistline is over 31.5 inches (80 cm) and men whose waist measures more than 37 inches (94 cm) should watch their weight.
- A waist size greater than 35 inches (89 cm) in women and 40 inches (102 cm) in men is associated with a higher risk for heart disease, diabetes, and impaired health.
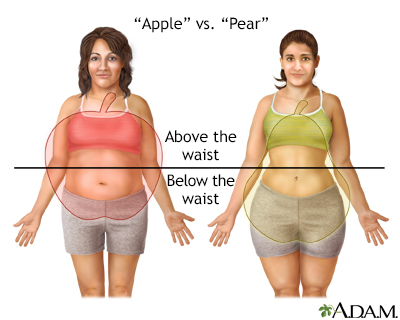
Excess body fat around the abdomen (the apple shape or android fat distribution) is a more consistent predictor of heart problems and health risks than BMI.
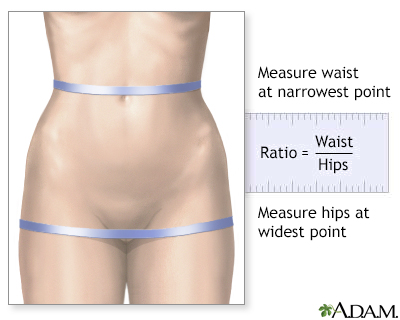
Waist-Hip RatioThe distribution of fat can be evaluated by dividing waist size by hip size. For example, a woman with a 30-inch (76 cm) waist and 40-inch (102 cm) hip circumference would have a ratio of 0.75; a woman with a 41-inch (104 cm) waist and 39-inch (100 cm) hips would have a ratio of 1.05. The lower the waist-hip ratio, the better. The risk of heart disease rises sharply for women with ratios above 0.85 and for men with ratios above 1.0.
Anthropometry
Anthropometry is the measurement of skin fold thickness in different areas, particularly around the triceps, shoulder blades, and hips. This measurement is useful for determining how much weight is due to muscle or fat.
Dual-energy x-ray absorptiometryDXA is the most convenient and accurate method to measure the body composition. DXA takes only 10 to 20 minutes to scan whole body with very low radiation exposure.
Measurement of Obesity in Children
Measuring body fat and diagnosing obesity is different in children and adults. In children, the amount of body fat changes with age. Because of this, BMI is harder to interpret during puberty and periods of rapid growth. In addition, girls and boys normally have different amounts of body fat.
A BMI that indicates obesity at one age may be normal for a child of a different age. To determine if a child is overweight or obese, experts compare BMI levels of children of the same age. They use a special chart to decide whether a child's weight is healthy or not.
- If a child's BMI is higher than 85% of other children who are the same age and sex, they are considered at risk for being overweight.
- If a child's BMI is higher than 95% of other children the same age and sex, they are considered overweight or obese.
Causes
Many people with obesity who lose large amounts of weight and gain it back often think it is their fault. They may blame themselves for not having the willpower to keep the weight off, and many regain more than they lost.
Today, we know that biology is part of the reason some people cannot keep weight off. Even among people who live in the same environment and eat the same foods, some become obese and others do not. Our bodies have a complex system to help keep weight at a healthy level. In some people, this system may not work correctly.
Think about the gas gauge in your car. If the gas tank is full but the car's gas gauge is broken, it may read empty. You would want to put in more gas, even when the tank is already full.
Some people struggle to maintain a healthy weight because one or more of the signals that tells the brain when they have eaten enough does not work correctly. In other words, the gas tank (stomach) may be full, but the brain (gas gauge) does not realize that.
The Biological Pathway to Appetite
Appetite is determined by processes that occur both in the brain and gastrointestinal tract. Eating patterns are controlled by areas in the hypothalamus (in the brain).
The body produces a number of molecules that increase or decrease appetite.
Leptin is a hormone that decreases appetite by reducing neuropeptide Y (NPY, a hunger stimulant) and by increasing a-melanocyte-stimulating hormone (a-MSH, a food intake inhibitor). A short-term increase in leptin levels decreases appetite, whereas falling levels of leptin induce hunger. Leptin is produced by fat cells and its blood levels rise as obesity develops. But appetite is not suppressed in obese people, although their leptin levels are increased, probably due to leptin resistance.
Ghrelin is another hormone that controls appetite. Ghrelin is mostly secreted by stomach cells and it works by telling the brain when the stomach is empty, causing hunger pangs and a decrease in metabolism (gastric bypass surgery reduces the size of the stomach and decreases levels of ghrelin).
Other hormones involved in the feeling of satiety are cholecystokinin (CCK), glucagon-like peptide 1 (GLP-1), apolipoprotein A-IV, and polypeptide YY.
Specific Genetic Factors
Our bodies are set to maintain weight within a certain range. That weight range is at least partly determined by our genetic makeup. Genetic makeup refers to certain traits that we inherit from our parents. If a person has the genetic makeup for obesity and they eat a lot of high-calorie foods and do not exercise, it is almost certain they will become obese. It will likely be harder for such a person to stay at a healthy weight than someone who does not have the genes for obesity.
Obesity is not caused by just one gene. There are hundreds of genes that influence body weight. Some people have more genetic risk factors for obesity than others. However, scientists have not yet discovered the exact genes that contribute to obesity.
Learned Behaviors and Habits
The way we eat when we are children may strongly affect our eating behaviors as adults. When we repeat these behaviors over many years, they become habits. They affect what we eat, when we eat, and how much we eat.
Children are very good at listening to their body's hunger and fullness signals. They will stop eating as soon as their body tells them they have had enough. However, at some point a well-meaning parent may tell them they have to finish everything on their plate. This forces them to ignore their fullness and to eat everything that is served to them.
As adults, these same people may say they feel guilty if they do not eat everything on their plate. And today, portion sizes are so large that eating everything on your plate may mean you are eating too many calories.
Other learned behaviors include using food to:
- Reward good behaviors
- Seek comfort when feeling sad or stressed
- Express love
These learned habits lead to eating when someone is already full. Many people have a very hard time breaking these habits.
The foods we eat when we are children may influence our food likes and dislikes for life. Being raised on processed foods that are high in fat, salt, and sugar may make it difficult to start eating natural foods, such as fruits, vegetables, and whole grains, when we become adults. Not knowing how to prepare these foods can also keep people from eating them.
Television and Sedentary Habits
We are surrounded by many things that make it easy to overeat and hard to stay active.
Many people don't feel like they have enough time to plan and prepare healthy meals. This may be because they:
- Work outside the home
- Work long hours, or night shifts
- Have a long commute
Less free time also means less time to exercise. Also, more people today work desk jobs, compared to more active jobs in the past.
Devices such as remote controls, mobile telephones, escalators, elevators, and computers all make life easier for us. But fewer trips up and down stairs and fewer walks down the hall at work to talk with a co-worker mean that we are storing more calories instead of burning them off.
Researchers have found that labor-saving devices have reduced people's energy usage by over 100 calories a day. The average American now eats 100 to 200 more calories a day than they did 10 years ago. Less activity and more calories can lead to a weight gain of 12 to 25 pounds (5 to 11 kilograms) every year.
Long hours in front of a TV or computer may be the most hazardous pattern of behavior. TV watching produces a lower metabolic rate than sewing, playing board games, reading, writing, and driving a car. And many people engage in unhealthy snacking and eating patterns while watching TV.
Modern Diet and Eating Habits
Many things have changed how and what we eat. Some of these are:
- Children may see thousands of food commercials every year. Most of these are for candy, fast food, soft drinks, and sugared cereals.
- More foods today are processed or prepared outside of the home and may have excessive levels of added fat, sugar, or sodium.
- Vending machines and convenience stores make it easy to get a quick snack, but they rarely sell healthy foods.
- More people eat out, most often at food courts, fast-food restaurants, and all-you-can-eat buffets.
People are not only eating more food than they did 20 years ago, but they are also replacing home cooking with packaged foods, fast food, and dining out. Fast foods tend to be served in larger portions. They generally contain more calories and unhealthy fats, and fewer nutritious ingredients, than homemade or restaurant meals. Snack foods and sweet beverages, including juice and soft drinks, add to the increasing rates of obesity.
Medical or Physical Causes of Obesity
Several medical conditions may contribute to being overweight, but only rarely are they a primary cause of obesity.
- Hypothyroidism is sometimes associated with weight gain. However, patients with an underactive thyroid generally show only a moderate weight increase of 5 to 10 pounds (2 to 5 kilograms).
- Very rare genetic disorders, including Froehlich syndrome in boys, Laurence-Moon-Biedl syndrome, and Prader-Willi syndrome, cause obesity.
- Abnormalities or injury of the hypothalamus can cause obesity.
- Cushing disease is a rare condition caused by high levels of steroid hormones. It results in obesity, a moon-shaped face, and muscle wasting.
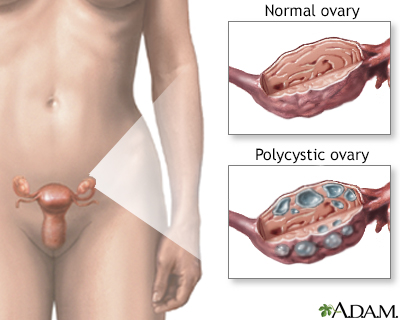
- Obesity is also linked to polycystic ovarian syndrome, a hormonal disorder in women.
Effects of Certain Medications
Some prescription medications may contribute to weight gain, usually by increasing appetite. Such drugs include:
- Corticosteroids.
- Female hormone treatments, including some oral birth control pills (the effect is usually temporary), and certain progestins (such as Megestrol) used to treat cancer.
- Certain antidepressants including fluoxetine, amitriptyline, and bupropion.
- Antiseizure medications, including topiramate, gabapentin, and valproate.
- Most antimanic and antipsychotic drugs, including lithium, risperidone, olanzapine, quetiapine, and others.
- Insulin and insulin-stimulating drugs used to treat diabetes, which causes problems for obese people with type 2 diabetes.
Do not stop taking any medications without first talking to your health care provider.
Risk Factors
Where you live plays a role in your risk for obesity. For example, simply living in the United States makes a person more susceptible to obesity. The prevalence of obesity in America has risen dramatically over the past few years and continues to increase.
- According to the latest figures available, more than a third of American adults (ages 20 and older) are obese (BMI 30 or more) -- up significantly from the early 1990s.
- The number of Americans ages 20 to 74 who are overweight or obese also increased from below 50% in 1960 to 72% in 2016.
- Regionally, the prevalence of obesity is lowest in the Western states and highest in the South.
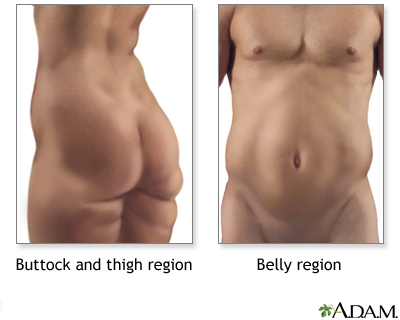
Fat tends to settle in certain regions, depending on gender. Women gain fat predominantly in the stomach, hips, and thighs, while men tend to gain fat in the belly and waist.
Risk by AgePeople of any age are at risk for obesity. More children and adolescents are overweight in America than ever before. Gaining some weight is common with age, and adding about 10 pounds (5 kilograms) to a normal base weight over time is not harmful. The typical weight gain in American adults over 50, however, is worrisome. By age 55, the average American has added nearly 40 pounds (18 kilograms) of fat during the course of adulthood. This condition is made worse by the fact that muscle and bone mass decrease with age.
Risk by GenderIn men, BMI tends to increase until age 50 and then it levels off. In women, weight tends to increase until age 70 before it plateaus. There are 3 high-risk periods for weight gain in women:
- The first is at the onset of menstruation, particularly if it is early.
- The second is after pregnancy, if weight that has been gained is not lost.
- Finally, many women gain 12 to 15 pounds after menopause.
Obesity is more prevalent in lower economic groups. Low-income people tend to eat fewer fruits and vegetables and take in more calories a day than higher-income people. However, obesity is increasing in college-educated young adults, as well as in other groups. Fast food may also be cheaper and more accessible for many, while fresh produce and healthy foods are often more expensive and harder to find.
Ethnic GroupsAmong ethnic groups in general, African-American women are more overweight than Caucasian women, but African-American men are less obese than Caucasian men. Hispanic men and women tend to weigh more than Caucasians.
Dietary Habits that Increase Risk
In many cases, lifestyle habits and patterns are so well-established and automatic that people are not even aware they are bad for health.
A number of dietary habits put people at risk for becoming overweight:
- Night-eating syndrome is when people have no appetite in the morning, stay awake at night (have insomnia), and consume more than half of their daily food intake after 6 p.m. It is associated with obesity and is difficult to treat.
- About 30% of people who are obese are binge eaters who may consume up to 5000 to 15,000 calories in one sitting.
Specific Groups at Risk
Anyone with a Sedentary LifestyleOffice workers, drivers, and people who sit for long periods are at higher risk for obesity.
Ex-SmokersNicotine increases the metabolic rate, and quitting, even without eating more, can cause weight gain. Most people who quit smoking gain 4 to 10 pounds (2 to 5 kilograms) in the first 6 months after quitting. Some gain as much as 25 to 30 pounds (11 to 14 kilograms). It is important to note that weight control is not a valid reason to smoke.
People with DisabilitiesObesity rates are higher than average in people with physical or mental disabilities. Those with disabilities in the lower part of the body, such as the legs, are at highest risk.
People with Chronic Mental illnessesPeople who have a chronic mental illness are at high risk for obesity and diabetes, most likely due to their lifestyle. In addition, many of the medications used to treat chronic mental illnesses can cause weight gain and increase the risk of diabetes.
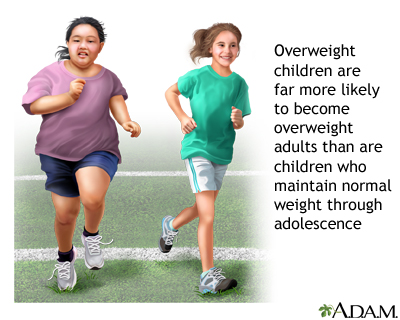
Overweight Children: Special Considerations
Obesity has become a serious health problem in children and teenagers. A child who is overweight or obese is more likely to be overweight or obese as an adult.
Obese children are now developing health problems that used to be seen only in adults. When these problems begin in childhood, they often become more severe when the child becomes an adult.
Today 18% of children (ages 6 to 11) and 21% of adolescents (ages 12 to 19) are obese. The number of obese children and adolescents has more than tripled since the 1980s.
Children and adolescents- Percent of adolescents age 12 to 19 years with obesity: 20.6% (2015-2016)
- Percent of children age 6 to 11 years with obesity: 18.4% (2015-2016)
- Percent of children age 2 to 5 years with obesity: 13.9% (2015-2016)
No single factor or behavior causes obesity. Obesity is caused by the many factors described above, including a person's habits, lifestyle, and environment. Genetics and some medical conditions also increase a person's chances of becoming obese.
Children are surrounded by many things that make it easy for them to overeat and harder to be active:
- Parents have less time to plan and prepare healthy meals. As a result, children are eating more packaged and fast foods that are usually less healthy than home-cooked meals.
- Vending machines and convenience stores make it easy to get a quick snack, but they rarely sell healthy foods.
- Overeating is a habit that is reinforced by restaurants that advertise high-calorie foods and large portion sizes at low cost.
Biological Effect of Childhood Obesity on Adult Weight
Achieving a healthy weight becomes more difficult as children get older. The odds of obesity persisting into adulthood range from 20% in 4 years olds to 80% in teenagers. One reason for the persistence is biological. The fat cells change in number or mass depending on a person's age:
- Fat cells multiply during two growth periods: early childhood and adolescence. Overeating during those times increases the
number
of fat cells, which are then maintained in adulthood. - After adolescence, fat cells tend to increase in
mass
rather than quantity, so that adults who overeat and gain weight tend to have larger fat cells, not more of them. This growth in mass may be responsible for the greater risk of persistent obesity among teenagers compared to children who are overweight. Losing weight after adolescence reduces the size of fat cells but not their number, so weight loss becomes much more difficult.
Complications
Obesity is a medical condition in which a high amount of body fat makes it hard for a person's internal organs to work well. This can cause poor health. People with obesity are at risk for developing a number of health problems.
Three things can be used to determine if a person's body fat puts them at risk for developing obesity-related diseases:
- Body mass index (BMI)
- Waist size
- Other risk factors or chronic diseases
The higher the BMI, the greater the risk for certain diseases, such as heart disease, stroke, high blood pressure, type 2 diabetes, obstructive sleep apnea (pauses in breathing during sleep), and arthritis.
The risk of heart disease, hypertension, stroke, gout, and type 2 diabetes rises sharply for women with waist-hip ratios above 0.85 and for men with ratios above 1.0.
Weight gain in the area around the waist (apple type) is more dangerous than weight gained around the hips and flank area (pear type). Fat cells around the gut and abdominal organs (visceral fat) have different qualities than those found in the hips and thighs (subcutaneous fat).
Apple shape obesity is more commonly associated with insulin resistance and diabetes, high blood pressure, and unhealthy cholesterol and lipid levels.
General Adverse Effects of Being Overweight (Not Obese)Being overweight or obese is generally associated with a shorter lifespan. However, it is still not clear if being overweight (a BMI of 25 to 29.9) harms healthy people with no risk factors for serious illnesses.
The risk for developing type 2 diabetes, gallstones, hypertension, heart disease, stroke, and various cancers rises according to how much an individual is overweight. Adults who are overweight in middle age face a poor quality of life as they age, with the quality declining the more they weigh.
Some argue that unhealthy diet and sedentary lifestyle cause the harm -- not the extra weight itself -- in people who are not severely obese.
Being slightly overweight (versus underweight) may be linked with a lower risk of mortality in the elderly.
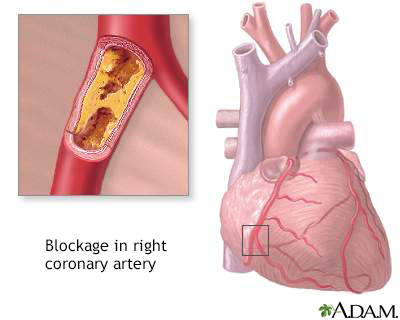
Heart Disease and Stroke
People who are obese have almost three times the risk for heart disease as people of normal weight. Being physically unfit adds to the risk.
Obesity poses many dangers to the heart and circulatory system:
-
Coronary artery disease and heart attacks
Coronary artery disease
An in-depth report on the causes, diagnosis, treatment, and prevention of coronary artery disease (CAD).
 Image
ImageRead Article Now Book Mark Article -
Heart failure
Heart failure
An in-depth report on the causes, diagnosis, treatment, and prevention of heart failure.
 Image
ImageRead Article Now Book Mark Article -
Stroke
Stroke
An in-depth report on the causes, diagnosis, treatment, and prevention of stroke.
 Image
ImageRead Article Now Book Mark Article
Obesity frequently associates with diabetes, high blood pressure, and obstructive sleep apnea, which all also increase the risk for stroke.
Insulin Resistance, Type 2 Diabetes, and Metabolic Syndrome
Type 2 Diabetes and Insulin ResistanceMost people with type 2 diabetes are overweight or obese, and weight loss may be the key to controlling the current epidemic of type 2 diabetes. The common factor appears to be insulin resistance -- that is, the body can no longer respond properly to insulin. This has the effect of increasing sugar levels in the blood, the hallmark of diabetes.
Insulin resistance is also associated with high blood pressure and abnormalities in blood clotting. Some research indicates that obesity is the one common element linking insulin resistance, type 2 diabetes, and high blood pressure.
Type 2 diabetes
An in-depth report on the causes, diagnosis, treatment, and prevention of type 2 diabetes.

| Read Article Now | Book Mark Article |
Metabolic syndrome (also called syndrome X) is a cluster of conditions that is significantly associated with heart disease and higher mortality rates from all causes. The syndrome consists of obesity marked by abdominal fat, unhealthy cholesterol levels, high blood pressure, and insulin resistance.
Cancer
The American Cancer Society's (ACS) cancer prevention guidelines stress the importance of keeping a healthy weight throughout life. The ACS indicates that healthy weight is even more important than eating specific healthy foods when it comes to cancer prevention.
Obesity has been associated with a higher risk for cancer in, general and specific cancers in particular. Studies have also suggested that restricting calories reduces the risk for cancer.
One way in which obesity may increase the risk for cancer is its association with high levels of hormones called growth factors, which can trigger rapid cell production, leading to cancer.
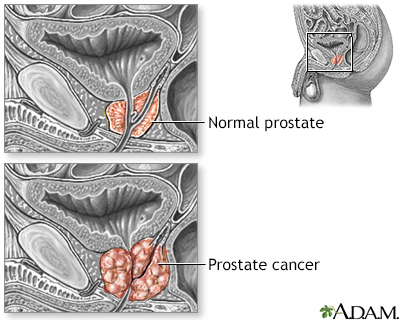
Obesity increases the risk of these cancers:
- Uterine cancer
- Breast cancer
- Prostate cancer
- Cancer of the esophagus
- Colon cancer
- Pancreatic cancer
Joints
More weight puts pressure on the bones and joints. This can lead to osteoarthritis, a disease that causes joint pain and stiffness. People who are obese are also at higher risk for carpal tunnel syndrome and other problems involving nerves in their wrists and hands. Overweight individuals with knee osteoarthritis benefit from diet and exercise programs for weight loss, which can lead to less knee pain, and improved function and quality of life.
Reproductive and Hormonal Problems
InfertilityAbnormal amounts of body fat, either 10% to 15% too high or too low, can contribute to infertility in women. Obesity is especially related to certain infertility problems, such as uterine fibroids and menstrual irregularities. In men, obesity can contribute to reduced testosterone levels and erectile dysfunction.
Effect on PregnancyObesity has many dangerous effects on pregnancy. These include a greater risk of developing high blood pressure, gestational diabetes (diabetes, usually temporary, that occurs during pregnancy), urinary tract infections, blood clots, prolonged labor, and higher fetal death rate in late stages of pregnancy. Obesity is also associated with increased rates of cesarean delivery. Infants of women who are obese are also at higher risk for neural tube birth defects, which affect the brain or spine, as well as other birth defects. Folic acid supplements, which are normally effective in preventing these conditions, may not be as protective in overweight women. Some evidence also suggests an association between obesity and stillbirths.
Effects on the Lungs
Obesity, especially moderate or severe obesity, also puts people at risk for hypoxia, a condition in which there is not enough oxygen to meet the body's needs. Obese people need to work harder to breathe. Their breathing muscles and lungs often do not work as well as those in thinner people.Pickwickian syndrome, named for an overweight character in a Dickens novel, occurs in severe obesity when a lack of oxygen produces intense and chronic sleepiness and, eventually, heart failure.
Effect on the Liver
Nonalcoholic Fatty Liver DiseasePeople with obesity, particularly if they also have type 2 diabetes, are at higher risk for a condition called nonalcoholic fatty liver disease (NAFLD), also called nonalcoholic steatohepatitis (NASH). This condition can cause liver damage that is similar to liver injury seen in alcoholism. NAFLD occurs in about 80% of people with type 2 diabetes, and 90% of people with high risk obesity. NASH can also occur in overweight children.
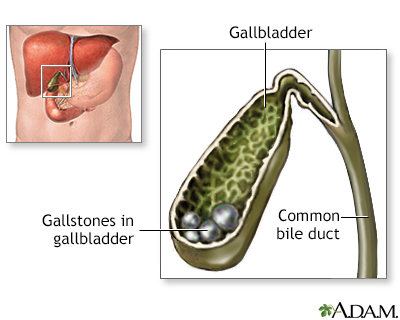
GallstonesThe incidence of gallstones is significantly higher in people with obesity. The risk for stone formation is also high if a person loses weight too quickly. In people on ultra-low-calorie diets, taking ursodeoxycholic acid (Actigall) may prevent gallstones.
Sleep Disorders
People who are obese and who nap tend to fall asleep faster and sleep longer during the day. At night, however, it takes them longer to fall asleep, and they sleep less than people of normal weight. Studies have suggested that obesity not only interferes with sleep, but that sleep problems may actually contribute to obesity.
Obstructive Sleep ApneaObesity, particularly the apple shape, is strongly associated obstructive with sleep apnea, which occurs when the upper throat relaxes and closes from time to time during sleep. This closure temporarily blocks the passage of air. Obstructive sleep apnea is increasingly being viewed as a potentially serious health problem, which may lead to complications such as heart disease and stroke. Weight loss is often recommended to treat obstructive sleep apnea. Bariatric surgery is no better than conventional weight loss programs in managing obstructive sleep apnea.
Obstructive sleep apnea may also increase obesity. Some studies indicate that treating obstructive sleep apnea may help people lose abdominal fat.
Emotional and Social Problems
DepressionSeveral studies have reported an association between depression and obesity, particularly in obese women. There may be a number of factors to explain the link. In some cases of atypical depression, people overeat and may gain weight. Overweight people may also become depressed because of social problems and a poor self-image.
There does not appear to be any association between depression and obesity in men.
Social ProblemsOne long-term study reported that overweight young women completed fewer years of school, were 20% less likely to be married, and had 10% higher rates of household poverty than their thinner peers. Obese young men were also less likely to be married, and their incomes were lower than their thinner peers. Nevertheless, studies consistently show that overweight males (both boys and men) are not as severely emotionally affected as females of any age. Women and girls tend to blame themselves for being heavy, while males tend to blame being overweight on outside factors.
Health Consequences of Childhood Overweight
Children and adolescents who are overweight have poorer health than other children. Studies are reporting unhealthy cholesterol levels and high blood pressure in overweight children and adolescents. Of great concern is the dramatic increase in type 2 diabetes in young people, which is largely due to the increase in overweight children.
Weight gain in children is also linked to asthma, gallbladder problems, sleep apnea, and liver abnormalities. Overweight girls seem more likely to enter puberty early, and subsequently to be at higher risk for breast cancer. It is not yet clear how many of these childhood problems persist in people who achieve normal weight as adults. Staying overweight into adulthood carries health risks.
Lifestyle Changes and Psychosocial Treatments
For most people, changing behavior takes time. All the stages of change are important. A person can learn from each stage. One can go from "not thinking about it" to "thinking about the pros and cons" to "making small changes and figuring out how to deal with the hard parts" to "doing it" to "making it part of your life." Many people fall off track and go through the stages of change several times before change really lasts.
Lifestyle changes usually involve slip-ups. People should not give up because they slip from time to time. Instead, they should forgive mistakes and get back to work toward the goal of lifelong health.
Keeping a Food Journal
A food journal is a good way to become aware of eating habits.
- Keep a food journal for 1 week. Write down what you eat, how much you eat, and what time of day you've eaten. Also write down what else you were doing and how you were feeling, such as being hungry, stressed, tired, or bored. For example, maybe you were at work and were bored, so you got a snack from a vending machine down the hall from your desk.
- At the end of the week, review your journal and look at your eating habits. Try to decide which habits you want to change. Remember: small steps can lead to long-term success. Try not to overwhelm yourself with too many goals.
- Also, congratulate yourself for the healthy habits you do have. Many people focus on their poor habits and then become distressed and overwhelmed. Don't judge your behaviors. Setting goals to correct flaws is the best way to make new healthful habits permanent.
Think about what triggers, or prompts some of your eating habits. Is there something in your environment, such as a vending machine down the hall, that makes you eat when you are not hungry or choose an unhealthy snack? Does the way you feel make you want to eat?
Look at your journal and circle the common triggers. Some of them might be:
- Seeing your favorite snack in the pantry or vending machine
- Watching television
- Feeling stressed by something at work or by another situation
- Having no plan for dinner after a long day
- Going to a staff meeting to which someone brought cupcakes
- Stopping at a fast-food restaurant for breakfast and choosing high-fat, high-calorie foods
- Needing a pick-me-up toward the end of your workday
Avoiding Triggers to Overeating
Start by focusing on the one or two triggers that occurred the most often during your week. Is there something you could do to avoid these triggers?
Some ways to avoid triggers are:
- Don't walk past the vending machine to get to your desk, if possible.
- Decide what you will have for dinner early in the day so that you have a plan after work.
- Keep unhealthy snacks out of your house or ask the person in your home who buys these snacks to keep them out of sight.
- Suggest having fruit and vegetables in place of cupcakes at staff meetings, or bring these things yourself.
Replacing old Habits with New, Healthy Ones
Some other ideas for replacing unhealthy habits with healthy ones are:
- Eat slowly. Eating too quickly leads to overeating.
- Eat only when you are hungry. Eating when you are feeling worried, tense, or bored also leads to overeating.
- Plan your meals. This reduces the chance you will buy foods you did not plan to buy (impulse buying) or eat at fast-food restaurants.
- Control your portion sizes.
- Add more low-starch vegetables to your meals and snacks.
- Get rid of unhealthy foods. Replace the candy dish with a fruit or nut bowl. If you must have tempting, unhealthy foods in your house for other family members, put them out of sight on a high shelf or at the back of the cupboard.
- Avoid skipping meals. Eat breakfast like a king or queen, lunch like a prince or princess, and dinner like a pauper.
It may take a while to turn unhealthy habits into new, healthy ones. Since it took a while to form the old habits, it may take just as long to change them. Do not give up.
Managing Overweight Children
Childhood obesity is best treated by a non-drug, multidisciplinary approach, including diet, behavior modification, and exercise. Children should be screened for obesity at age 6, and referred to weight management programs if needed at that time. Moderate-to-intense programs have the highest rate of success with children and adolescents. These programs include counseling and behavior modifications.
Most children spend about 3 hours a day watching TV. When you add in other screen time activities, they spend closer to 5 to 7 hours a day. Current screen time guidelines recommend that children under age 2 have no screen time. Above age 2, children should limit screen time to 1 to 2 hours a day.
Children should have many chances to run, bike, and play sports during the day. CDC recommends that children age 2 and older get 60 minutes of activity every day. The activities should comprise of moderate to vigorous aerobic exercises. Some examples are:
- Walking briskly
- Playing chase or tag
- Playing basketball or other organized sports (such as soccer, track, or swimming)
Younger children have shorter attention spans than older children. They may be active for only 10 to 15 minutes at a time. The goal is still a total of 60 minutes of activity every day. These ideas may help non-athletic children become active:
- Let them know it will give them more energy, make their bodies stronger, and make them feel good about themselves.
- Encourage them to be active, so they know they can do it. They need to believe they can.
- Be their role model. If you are not active yourself, start getting more active. Make walking a part of your family's daily routine. All you need are good walking shoes and rain jackets for the wet days. Don't let rain stop you. Go for walks together after dinner, before turning on the TV or playing computer games.
- Take your family to community centers or parks where there are playgrounds, ball fields, basketball courts, and walking paths. It's easier to be active when people around you are active.
Choosing healthy snacks and drinks for your children can be a challenge. There are many to choose from.
- Put snacks in small plastic bags so they are easy to carry in a pocket or backpack. Putting snacks in small bags also helps you give your child the right portion size.
- Avoid junk-food snacks like chips, candy, cake, cookies, and ice cream. The best way to keep kids from eating junk food or other unhealthy snacks is to not have these foods in your house.
- Teach them how to avoid unhealthy foods at school.
- It's okay to let your child have an unhealthy snack once in a while. Never allowing any unhealthy snacks or sweets may result in your child sneaking these foods. The key is balance.
- Praise and reward children when they make good food choices and do healthy activities. This will encourage them to keep at it.
- Do not use food as a reward or punishment. For instance, do not offer food if your children clean their rooms, and do not withhold food if your children do not do their homework.
- Do not punish, tease, or put down children who are not motivated in their weight-loss plan. This will not motivate them.
- Do not force children to eat all the food on their plate. Infants, children, and teens need to learn to stop eating when they are full.
The best thing parents can do to motivate their kids to lose weight is to lose weight themselves, if they need to. Parents should lead the way and follow the advice they give their children.
Eating as a family is important. Have meals where everyone sits down and talks about their day. These meals should have some set rules, such as no lectures or teasing allowed. Family meals should be a positive experience. Meals should be cooked at home, and children should be involved in the meal planning. If they are old enough, they can help prepare meals.
Teaching parents healthy lifestyle skills may lead to a sustained weight reduction in moderately-obese children. More research is needed, however, to assess the benefits of home-based programs for the prevention of childhood obesity.
Support Groups and Behavioral Approaches
Commercial and Nonprofit Support Programs for Weight LossThere are many different types of weight-loss programs. (This report cannot address all of the many commercial and nonprofit weight-loss programs currently available, nor can it assess their claims.)
Taking off Pounds Sensibly (TOPS), a nonprofit support organization with many local chapters, is one of the least expensive programs in the United States.
Most commercial programs, such as Weight Watchers, Jenny Craig, and NutriSystem, offer individual or group support, lifestyle changes, and packaged meals. These programs tend to be more expensive. There are few well-conducted studies on these programs.
Approach short-term goals regarding exercise and eating as something to learn, rather than perform. Also, plan ahead when eating out or at someone else's home.
Cognitive Behavioral ApproachesMost support programs use some form of cognitive behavioral methods to change the daily patterns associated with eating. They are very useful for preventing relapse after initial weight loss.
In these programs, you review a personal diary with a therapist or group to set realistic goals and identify patterns you can change. For instance, if you normally eat food while watching television, you may need to eat in another room instead.
Stress-Reduction TechniquesStress reduction and relaxation techniques may be helpful for some people with obesity, such as those whose weight is related to night-eating syndrome.
Stress reduction and relaxation techniques
An in-depth report on the causes, diagnosis, treatment, and prevention of stress.
| Read Article Now | Book Mark Article |
Changing Sedentary Habits and Exercise
The weight-loss formula: calories used (including exercise) > calories eaten = weight loss.
This means that to lose weight, the number of calories you burn needs to be greater than the number of calories you get from foods and drinks. Even if you work out a lot, you will gain weight if you take in more calories than you burn.
For example, a 30- to 50-year-old woman of average normal weight who does not exercise needs about 1800 calories a day to maintain her weight. A 30- to 50-year-old man of average normal weight who does not exercise needs about 2200 calories to maintain his weight. For every hour of exercise they do, they will burn approximately:
- 240 to 300 calories doing light activity, such as cleaning house or playing baseball or golf.
- 370 to 460 calories doing moderate activity, such as a brisk walk (3.5 mph), gardening, biking (5.5 mph), or dancing.
- 580 to 730 calories doing strenuous activity, such as running at a pace of 9 minutes per mile, playing football, or swimming laps.
- 740 to 920 calories doing very strenuous activity, such as running at a pace of 7 minutes per mile, playing racquetball, or skiing.
Even without dieting, people will lose weight if they add any of these activities to their lifestyle. Doing strength-training can help to build/maintain lean body mass, which can help to increase the amount of calories your body uses throughout the day.
Many people sit all day at their jobs. They can add activity to their schedule before work, during work, at lunch, and after work.
- People who drive can park around the corner or a few blocks from their workplace to get in a 5- to 10-minute walk before work.
- People who take the bus or train can get off 1 stop before their usual stop to get in a few extra minutes of walking.
- Walking or biking to work are excellent forms of exercise that save money on parking, gas, and bus fare.
- People with sedentary jobs should set a timer to remind them to do 1 minute of stretching or strengthening exercises every half hour. These 1-minute workouts help people stay focused, and they add 16 minutes of exercise to an 8-hour workday.
- Take the stairs instead of the elevator to add some exercise to the workday. Walk down the hall to talk with a co-worker instead of sending an e-mail.
- People who get an hour lunch break can eat for 30 minutes, then take a 30-minute walk.
- Those who get a 30-minute lunch can try to fit in a 10-minute power walk.
People who exercise are more apt to stay on a diet plan. Exercise improves psychological well-being and replaces sedentary habits that usually lead to snacking. Exercise may even act as a mild appetite suppressant. Moreover, exercise improves overall health, even with only modest weight loss.
Be aware, however, that the pounds won't magically melt off. If a person exercises but doesn't diet, any actual pounds lost may be minimal due to simultaneous gain of muscle mass. But regardless of weight loss, a fit body will be healthier and will look more toned. In addition, exercise benefits the heart and vascular system and raises HDL (good) cholesterol levels, even with no weight loss.
The following are some suggestions and observations on exercise and weight loss:
- With intense exercise, the metabolism continues to burn calories before returning to its resting level. This state of elevated metabolism can last for as little as a few minutes after light exercise to as long as several hours after prolonged or heavy exercise.
- Of the standard aerobic machines, the treadmill burns the most calories. It may be particularly effective when used in multiple short bouts during the day. Frequent, short exercise sessions of as little as 10 minutes each (about four times a day) may be the most successful exercise program for obese people.
- Resistance or strength training builds muscles. It should be performed 2 or 3 times a week.
- As people slim down, physical activity becomes easier and they burn fewer calories for the same amount of work. The rate of weight loss slows down, sometimes discouragingly so. Be aware of this phenomenon and keep increasing and varying your daily exercise program.
- Changes in fat and muscle distribution may differ between men and women. Men tend to lose more abdominal fat than women. In one study, women in aerobic and strength training programs lost fat in their arms and trunk, but did not gain muscle tissue in these regions.
Because obesity is one of the risk factors for heart disease and diabetes, anyone who is overweight should discuss their exercise program with a doctor before starting.
Exercise program
An in-depth report about the benefits and types of exercise.

| Read Article Now | Book Mark Article |
Dietary Management
About 50 to 70 million Americans go on diets each year. No one diet is right for everyone. What works for one person may not work for another.
Before beginning a diet, look at your own eating and activity patterns. Then set goals for changing some of these patterns or behaviors. Set goals that are realistic for you; goals that you can reach and maintain.
A good diet is one you can follow for years. It is better to make moderate lifestyle changes than attempt severe short-term changes. It should keep your weight at a good level for you and keep you in good health. Some key features of any good weight-loss program or diet are:
- The diet should be balanced. That means eating a variety of foods, including fruits and vegetables, healthy carbohydrates, proteins, and fats.
- The diet should not be boring or keep you on the same food for long periods of time. Although a weight-loss diet may limit some of the foods you enjoy eating, you should still enjoy eating.
- Weight loss should be gradual. Claims of quick and easy sustained weight loss are rarely true. The truth is it takes time, effort, and motivation to lose weight and keep it off.
- The exact composition of a diet is generally less important than the calorie reduction it supplies.
Be cautious about any diet that:
- Makes unrealistic claims about how much weight you can expect to lose.
- Tells you not to eat food from one of the major food groups.
- Is based on eating just one food or one type of food.
- Does not have any evidence or nonbiased research to support its claims.
Keeping Track of Calories
Calorie restriction has been the cornerstone of obesity treatment.
As a rough rule of thumb, one pound (450 grams) of pure body fat is the result of eating about 3500 calories. A person could lose a pound a week by reducing daily caloric intake by about 500 calories a day.
The calorie requirements for sustaining basal metabolism can be accurately determined by indirect calorimetry. It can also be estimated using formulas such as the Mifflin St Jeor equation, considered the most accurate in estimating calorie needs for obese people. Calorie requirements for maintenance of weight or for weight loss depend on current weight, gender, age, and activity levels.
For instance:
- A 50-year-old woman who is 5'1 (1.56 m) tall and wants to maintain a weight of 135 pounds and is mildly active might require only 12 calories per pound (1620 calories a day).
- A 25-year-old female athlete of the same height who wants to maintain the same weight might need 25 calories per pound (3375 calories a day).
Fat intake should be no more than 30% of total calories. Most fats should be in the form of monounsaturated and polyunsaturated fats (such as olive oil or fish oil). Avoid saturated fats (found in animal products such as lard or butter).
Warning on Extreme Diets
Extreme diets of fewer than 1100 calories per day carry health risks and are not recommended. Most of the initial weight loss is in fluids. Later, fat is lost, but so is muscle, which can account for more than 30% of the weight loss. No one should be on a very strict diet for longer than 16 weeks, or fast for weight loss.
There are a number of problems associated with extreme diets:
- They are often followed by bingeing or overeating, and a return to the weight prior to the diet, or even an increase in weight.
- Such diets often do not supply enough vitamins and minerals, which must then be taken as supplements.
- Severe dieting has unpleasant side effects, including fatigue, dizziness, confusion, intolerance to cold, hair loss, gallstone formation, and menstrual irregularities.
- There have been rare reports of death from heart arrhythmias when people drank liquid diet formulas that did not contain sufficient nutrients.
Pregnant women who excessively diet during the first trimester put their unborn children at risk for birth defects. Not gaining appropriate weight during pregnancy puts the fetus at risk for life-long health issues.
Eat A Healthy Diet to Lose Weight
Eating a balanced diet means you consume the right types and amounts of foods and drinks to keep your body healthy.
For protein in the diet, choose:
- Meats that have been steamed, baked, or broiled rather than fried.
- Poultry with the skin removed.
- Lean cuts of beef or pork, such as round, top sirloin, or tenderloin (trim away any visible fat).
- Fish or shellfish. Although red meat does not have a specific influence on body weight, evidence suggests that a high consumption of red and processed meats is linked to cancer and other serious health problems.
- Pulses such as pinto beans, black beans, kidney beans, lentils, split peas, or garbanzo beans.
- Nuts and seeds, including almonds, hazelnuts, mixed nuts, peanuts, peanut butter, sunflower seeds, and walnuts. But watch how much you eat.
- Tofu, tempeh, and other soy-protein products.
Consume 3 cups per day of fat-free or low-fat milk or milk products. Items such as cream cheese, cream, or butter do not count as healthy dairy products.
Grain products include any food made from wheat, rice, oats, cornmeal, barley, or another cereal grain. Products made with grains can include pasta, oatmeal, breads, breakfast cereals, tortillas, and grits.
Grains are divided into either whole grains or refined grains. The key to eating healthy is to choose mostly whole-grain products.- Examples of whole grains are whole-wheat flour, bulgur (cracked wheat), oatmeal, whole cornmeal, and brown rice. To make sure you are buying or eating whole-grain products, look for words such as "whole grain" or "100% whole wheat."
- Refined grains have been treated to extend their shelf life and give them a finer texture. However, this process takes out fiber, iron, and many B vitamins. Limit foods that are made with refined grains, such as crackers, corn tortillas, most ready-to-eat cereals, and white rice.
Eat 2 cups (4 servings) of fruit and 2 1/2 cups of vegetables (5 servings) per day for an average 2000-calorie daily diet.
- Fruits and vegetables are low in calories. They are also packed with fiber, vitamins, and minerals. Eating a diet that is rich in fruits and vegetables can help you control your weight. It may also reduce your risk of cancer and other diseases.
- Because fruits and vegetables are high in fiber and water, they fill you up. Replace high-calorie foods with fruits and vegetables to reduce the amount of calories and fat in your diet without making you feel hungry.
Low-Carbohydrate Diets
Low carbohydrate diets generally restrict the amount of carbohydrates but do not restrict protein sources.
The Atkins diet restricts complex carbohydrates in vegetables and, particularly, fruits that are known to protect against heart disease. The Atkins diet can cause excessive calcium excretion in the urine, which increases the risk for kidney stones and osteoporosis. This is a weight loss diet and not designed for long term health.
Low-carb diets, such as South Beach, The Zone, and Sugar Busters, rely on a concept called the glycemic index, or GI, which ranks foods by how high and how quickly they cause blood sugar levels to rise. Foods on the lowest end of the index take longer to digest. Slow digestion wards off hunger pains. It also helps stabilize insulin levels. Foods high on the glycemic index include bread, white potatoes, and pasta, while low-glycemic foods include whole grains, fruit, lentils, and soybeans. Another fad low-carbohydrate diet is the ketogenic (keto) diet, which emphasizes a high fat consumption to push energy metabolism from glucose towards fatty acids. The keto diet may be considered therapeutic for certain neurologic conditions, such as refractory epilepsy in children. However, this diet greatly increases cholesterol blood levels, and therefore may increase the risk of heart disease and stroke. The keto diet is not clinically recommended as a method for weight loss, for long term health maintenance, or for any condition outside of clinical supervision.
There has been debate about whether Atkins and other low-carbohydrate diets can increase the risk for heart disease, because people who follow these diets tend to eat more saturated fat and animal protein and less fruits and vegetables. In general, these diets appear to lower triglyceride levels and raise HDL (good) cholesterol levels. Total cholesterol and LDL (bad) cholesterol levels tend to remain stable or possibly increase somewhat. However, large studies have not found an increased risk for heart disease, at least in the short term. In fact, some studies indicate that these diets may help lower blood pressure -- another heart disease risk.
Low-carbohydrate diets help with weight loss in the short term, possibly even better than low-fat, normal carbohydrate diets. However, overall, there isn't good evidence showing the long-term effectiveness of low-carbohydrate diets. Their long-term safety and other possible health effects are still a concern, especially since these diets restrict healthy foods, such as fruit, vegetables, and grains, and they don't restrict saturated fats.
Fat and Sugar Substitutes
Replacing fats and sugars with substitutes may help many people who have trouble maintaining their weight.
Fat SubstitutesFat substitutes added to commercial foods or used in baking deliver some of the desirable qualities of fat, without adding as many calories. They cannot be eaten in unlimited amounts, however, and are considered most useful for helping keep down total calorie count.
Olestra (Olean) passes through the body without leaving behind any calories from fat. Studies suggest that it helps improve cholesterol levels and may help overweight people lose weight. Early reports of cramps and diarrhea after eating food containing olestra have not proven to be significant. Of greater concern is the fact that even small amounts of olestra deplete the body of certain vitamins and nutrients that may help protect against serious diseases, including cancer. The FDA requires that the missing vitamins, but not other nutrients, be added back to olestra products.
Beta-glucan is a soluble fiber found in oats and barley. Products using this substance (Nu-Trim) may reduce cholesterol and have additional health benefits.
A number of other fat-replacers are also available. Although studies to date have not shown any significant adverse health effects from these products, their effect on weight control is uncertain, since many of them may be high in sugar. People who learn to cook using foods that are naturally lacking or low in fat will eventually lose their taste for high-fat foods, but the same may not be true for people who use fat substitutes.
Artificial SweetenersMany artificial or low-calorie sweeteners are available. Yet using these artificial sweeteners should not give dieters a license to increase their fat intake. There has been some concern about the chemicals used to produce many of these sweeteners. Natural low-calorie sweeteners may be more acceptable to many people.
- Saccharin (Sugar Twin, Sweet'N Low, Sucaryl, and Featherweight). Saccharin has been used for years. Saccharin should not be used during pregnancy due to the possibility of slow fetal clearance.
- Aspartame (Nutra-Sweet, Equal, and NutraTase). People with phenylketonuria (PKU), a genetic condition, should not use it. Studies have not reported any serious health dangers in otherwise healthy individuals.
- Sucralose (Splenda). Sucralose has no bitter aftertaste and works well in baking, unlike other artificial sweeteners. It is made from real sugar by replacing part of the sugar with chlorine. Some people are concerned because chlorinated molecules used in major industrial chemicals have been associated with cancer and birth defects. Over 100 studies have been conducted on sucralose over a 20-year period, with no reports of such risks.
- Acesulfame-potassium (Sweet One, SwissSweet, and Sunette). It has been used in the U.S. since 1988 with no reported side effects.
- Neotame (Neotame). Neotame is a synthetic variation of aspartame, which was developed to avoid aspartame's side effects. The association with aspartame has raised some concerns, but studies on Neotame to date have reported no alarming effects, and it appears to be safe for general consumption.
- D-tagatose (Tagatose). This reduced-calorie sweetener is made from lactose, which is the sugar found in dairy products and other foods. It may be especially beneficial for people with type 2 diabetes. It may also have additional benefits that help the intestinal tract.
- Alitame (Aclame) is formed from amino acids, the building blocks of proteins. It has the potential to be used in all products that contain sugar, including baked goods.
- Stevioside (Stevia). This is a natural sweetener derived from a South American plant. It is available in health food stores. People with diabetes should avoid alcohol-based forms. It has not been carefully tested.
Other sugar substitutes being investigated include glycyrrhizin (derived from licorice) and dihydrochalcone (derived from citrus fruits).
Liquid Meal Replacements
Some studies have reported good success with meal replacement beverages (such as Slim-Fast and Sweet Success). They contain major nutrients needed for daily requirements. Each serving typically contains 200 to 250 calories and replaces one meal. (Note: Using these replacement products for all meals severely reduces calories and can be harmful.)These weight loss programs can be costly. People who complete these programs may lose close to 10% of their weight in the short term. But many people regain over half of the lost weight over time.
Medications
There are several different drugs used for weight loss. Unless specifically instructed by a doctor, people should use non-drug methods for losing weight. Except under rare circumstances, pregnant or nursing women should never take diet medications of any kind, including herbal and over-the-counter remedies. While weight loss drugs in general have shown some benefit, the overall weight loss achieved is generally limited, generally around a 5% weight loss. In addition, people will usually regain the weight when they stop the medication.
Weight loss medications improve several risk factors for heart disease. However, use of obesity medication has not yet been shown to lower the risk for heart disease, stroke, and related problems. More research is necessary.
Over-the-Counter Weight Loss Products and Herbal Remedies
About 7% of American adults use nonprescription weight-loss products. People must be cautious when using any weight-loss medications, including over-the-counter diet pills and herbal remedies. Buying unverified products over the Internet can be particularly dangerous.Green TeaSome studies have suggested that regular tea drinking is associated with lower weight, particularly in people who drink it for years. However, better evidence is needed to confirm the results.
Thermogenic Approach to Weight LossAn approach to weight loss called thermogenic (or hepatothermic) therapy is based on the claim that certain natural compounds have properties that enable the liver to increase energy in cells and stimulate metabolism. Theoretically, the result would be fat loss. Among the substances used in such products are EPA-rich fish oil, sesamin, hydroxycitrate, pantethine, L-carnitine, pyruvate, aloe vera, aspartate, chromium, coenzyme Q10, green tea polyphenols, DHEA derivatives, cilostazol, diazoxide, and fibrate drugs.
Nearly all the current over-the-counter dietary aids contain some combination of these ingredients. There is no evidence that any of these ingredients can produce weight loss, and some may even have harmful effects.Chromium is a common ingredient in many diet supplements (such as Xenadrine, Dexatrim, Acutrim Natural, and Twinlab Diet Fuel). It is claimed to specifically promote fat loss, rather than lean muscle loss. There is no proof that chromium helps with weight loss.
Warnings on Some Ingredients in Over-the-Counter Diet Products
Ephedra, Ephedrine, and Ma HuangThe FDA does not allow the sale of drugs that contain ephedrine. In May 2004, the FDA banned the sale of dietary supplements that contain ephedra (also called Ma Huang). Ephedra can cause serious side effects, including strokes and heart attacks.
Brazilian Diet PillThe FDA has warned consumers not to buy a product known as the Brazilian diet pill. This product is labeled as a dietary supplement, but it contains several chemicals found in powerful prescription drugs.
Conjugated Linoleic Acid (CLA)Conjugated linoleic acid is found in many dietary products. There is no evidence that it produces weight loss. Furthermore, there is some concern that CLA might increase insulin resistance and a dangerous inflammatory response in people with obesity.
TiratricolOver-the-counter products containing tiratricol, a thyroid hormone analogue, have been sold for weight loss. Such products may increase the risk for thyroid disorders, heart attack, and stroke. Tiratricol is also known as triiodothyroacetic acid or TRIAC.
Laxative Actions in Natural SubstancesMany dietary herbal teas contain laxatives, which can cause gastrointestinal distress. If overused, they may lead to chronic pain, constipation, and dependency. Rarely, dehydration and death have occurred. Some laxative substances found in teas include senna, aloe, buckthorn, rhubarb root, cascara, and castor oil.
Guar GumSome fiber supplements containing guar gum have caused obstruction of the esophagus and gastrointestinal (digestive) tract.
ChitosanChitosan, a dietary fiber from shellfish, prevents a small amount of fat from being absorbed in the intestine. Well-conducted studies have not found it to be effective. People who are allergic to shellfish should not take these supplements.
PlantainDietary remedies that list the ingredient plantain may contain digitalis, a powerful chemical that affects the heart. NOTE: This substance should not be confused with the harmless banana-like plant also called plantain.
FDA-approved Prescription Weight Loss Medications
Orlistat (Xenical)Orlistat (Xenical) works be inhibiting enzymes that digest fats and slowing the absorption of far in the intestine by about 30%. Orlistat can help about one-third of obese patients lose a modest amount of weight, and can help in long-term maintenance of weight loss. Most often, it is recommended as the first line drug therapy for obesity. The average weight loss attained with this drug is around 6 pounds (~3 kilograms). However, many people regain a significant portion of this weight within 2 years. While orlistat does not work for all patients, it can improve cholesterol levels, regardless of weight loss, as well as lower blood pressure.
Orlistat can cause gastrointestinal problems and may interfere with the absorption of the fat-soluble vitamins A, D, and E and other important nutrients. The FDA recommends taking a daily multivitamin supplement when using this drug.
The most unpleasant side effect is leakage of oily feces from the anus. Restricting fats can reduce this effect. People with bowel disease should probably avoid orlistat. Despite these side effects, most patients are able to tolerate this medicine. Severe liver disease and kidney injury has rarely been reported with orlistat.
There is an approved over-the-counter version of orlistat. Sold under the name Alli, it is available at half the prescription strength of Xenical. Those eager to use it should consider its cost and modest benefits compared with its side effects.
Other Long-Term Obesity MedicationsThe FDA also approved Qsymia (phentermine and topiramate), Contrave (bupropion and naltrexone) and Belviq (lorcaserin HCI) for use in obese adults with a BMI of 30 or greater, or for adults with a BMI of 27 or greater who also have a weight-related medical problem, such as type 2 diabetes, hypertension, or dyslipidemia. These drugs are to be used in conjunction with lifestyle measures of dieting and physical activity. Users may experience a weight loss of 3% to 5% or more in 12 weeks. If this weight loss does not occur, the medication should not be continued. Pregnant women and women who are planning to become pregnant should not take either of these drugs.
Liraglutide (Saxenda) is approved as the fifth available obesity drug in the United States. It is approved for use in people with a BMI of 30 or greater or when a medical problem such as high blood pressure, type 2 diabetes, or elevated cholesterol is present in people with a BMI of 27 or greater.
- The dose is higher when used for obesity than when used for treatment of type 2 diabetes only.
- The drug should be discontinued after 16 weeks if there has not been weight loss of at least 4%.
- This drug is administered by injection.
Psychostimulants
Phentermine and Other SympathomimeticsSympathomimetics are drugs that act like the stress hormone (and chemical messenger) norepinephrine. These medications act as stimulants in the brain. Some are approved for treating obesity, but only for short-term use of 12 weeks or less. Average weight loss has been in the range of 7 pounds (3 kilograms) over the short-term. These medicines include:
- Phentermine (Ionamin, Adipex-P, Fastin)
- Benzphetamine (Didrex)
- Phendimetrazine (such as Adipost, Bontril, Melfiat, Plegine, Prelu-2, and Statobex)
Surgery
Bariatric surgeries produce weight loss through 2 mechanisms:
- Restrictive mechanism, by creating a smaller stomach. As a result, the patient will feel full or satisfied with less food and will not be able to eat as much food as before.
- Malabsorptive mechanism, by rerouting the food around a portion of the small intestine, which normally helps break down food. As a result, the body will not absorb all the calories in the ingested food.
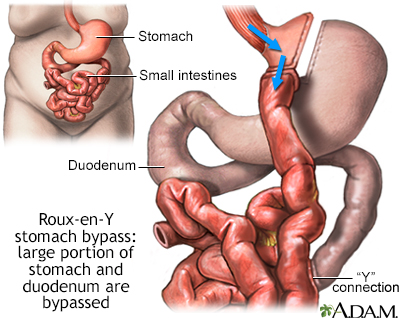
Gastric banding and sleeve gastrectomy are restrictive procedures. Biliopancreatic diversion is a malabsorptive procedure. Some bariatric surgeries are both restrictive and malabsorptive, including the gastric bypass and the duodenal switch procedures.
Gastric bypass (also called Roux-en-Y gastric bypass) creates a smaller stomach, but also reroutes or bypasses a portion of the small intestine. As a result, greater weight loss is achieved than with procedures that only create a smaller stomach.
The surgeries above are almost always done through laparoscopic approaches. This involves 5 to 6 small cuts in the abdomen for instruments and for a camera that allows the surgeon visual access.
Biliopancreatic diversion with a duodenal switch (BPD surgery) is more complex than other weight-loss surgeries and is done much less often -- usually only for severe, morbid obesity. The surgeon removes a large portion of the stomach and re-routes the passage of food so it does not pass through most of the small intestine, where food is normally absorbed (it is restrictive and malabsorptive).
Bariatric surgery requires specialized expertise and facilities. Studies have shown that the likelihood of complications is significantly associated with the experience of the surgeon and staff. A team approach with attention to dietary and metabolic needs is vital.
Benefits of Bariatric Surgery
Patients must still develop a healthy lifestyle and be calorie conscious after weight-loss surgery. Follow-up must be lifelong. Those who are able to change their lifestyle can expect to lose 30% to 50% of their excess weight, depending on the procedure.
Outcomes after gastric bypass surgery and sleeve gastrectomy are better than outcomes after gastric banding.
Bariatric surgery can reduce the risk of disease in people with severe obesity. These risks include type 2 diabetes, high blood pressure, heart disease, stroke, obstructive sleep apnea, arthritis, and some cancers. Successful weight loss after surgery can also lead to improvements in people who already have these conditions.
Losing weight should also make it much easier for the patient to move around and do everyday activities.
Weight-loss surgery alone is not a solution to losing weight. It can train you to eat less, but you still have to do much of the work. To lose weight and avoid complications from the procedure, you will need to follow exercise and eating guidelines from your doctor and dietitian.
Candidates for Bariatric Surgery
Surgery may be used for individuals who have been severely obese for 5 years or more and have not responded to other weight-loss therapies, such as diet, exercise, or medications.
Body mass index (BMI) is the most common measure of obesity. BMI measures weight in relation to height.
Doctors often use the following BMI measures to identify patients who may be most likely to benefit from weight-loss surgery:
- A BMI of 40 or greater. This usually means men are 100 pounds (40 kilograms) and women are 80 pounds (36 kilograms) over their ideal weight.
- A BMI of 35 or greater, along with a serious medical condition related to obesity. These are called
comorbidities
, and include such conditions as type 2 diabetes (high blood sugar), high blood pressure, osteoarthritis (severe), sleep apnea (sleepiness during the day and loud snoring, gasping, and interrupted breathing during sleep), and heart disease (personal or family history).
Some experts now support weight-loss surgery for most patients with a BMI of 30 or greater who have type 2 diabetes. Weight-loss surgery appears to produce better glucose control than medical therapy alone in patients with type 2 diabetes.
Your doctor must also consider medical problems that could make surgery more risky for you. These include:
- Liver or kidney disease
- Diseases of the stomach or small intestine
- Alcohol or substance abuse
- Current smoking
- Poorly controlled psychiatric or emotional problems
Patients with binge eating disorder should be identified and treated before surgery. A full evaluation, including a psychological evaluation, should be performed on all candidates for surgery.
Patients who are considering bariatric surgery should be well-informed regarding the procedure, its effectiveness, side effects, and complications. They should also understand the following:
- Lifestyle and behavioral changes will still be needed after surgery, including the need to focus on weight, chew food well, watch the diet, and take vitamin and mineral supplements.
- Patients will be unable to eat large meals.
- Surgery may not be successful at achieving significant weight loss.
Is weight-loss surgery safe for teens?
- Studies of adolescents who have had bariatric surgery suggest that these operations are at least as safe for adolescents as they are for adults. But not enough teenagers have been followed after their weight-loss surgery to know if there are any long-term effects on their future growth or development.
- Teenagers' bodies are still changing and developing. Because of the quick weight loss after surgery, they will need to be careful to get all the nutrients and vitamins their bodies require.
- Because gastric bypass surgery changes the way some nutrients are absorbed, teens who have weight-loss surgery will need to take certain vitamins and minerals for the rest of their life.
Laparoscopic Gastric Banding
In laparoscopic gastric banding, the surgeon places a band around the upper part of the stomach to create a small pouch to hold food. After surgery, the doctor can adjust the band to make food pass more slowly or quickly through your digestive system. The band around your stomach is filled with saline (saltwater). It is connected to a container (access port) that is placed under your skin in your upper belly. Your surgeon can make the band tighter or looser by increasing or decreasing the amount of saline in the band. To do this, your surgeon will insert a needle through your skin into the access port.
Most people go home the same day of surgery. Some will stay 1 night in the hospital. Most people take 1 week off of work.
The average weight loss is about one-third to one-half of your extra weight. This may be enough. The weight will usually come off more slowly than with gastric bypass. You should keep losing weight for up to 3 years.
The band is removable, if necessary. Studies to date indicate that the intestinal tract returns to normal afterward. Studies, including those done in the elderly, have reported significant weight loss and improved quality of life with the procedure.
Gastric Bypass (Roux-en-Y Gastric Bypass)
In gastric bypass, the stomach is divided with staples into two parts. The first part is very small, about the size of a golf ball. This small stomach is called the pouch. The second part of the stomach is much bigger, but food cannot go into it.
The small intestine is connected to the small pouch, which re-routes food around the big part of the stomach. The pouch can only hold a small amount of food, so if you eat too much or too fast you will throw up. Also, your body will not absorb all the calories in the food you eat.
Most people stay in the hospital for 2 days after open surgery. You may have a drain (tube) coming out of the stomach, which will drain fluids that build up after surgery. The drain tube is usually taken out about 7 to 10 days after surgery.
You may need to take 3 to 4 weeks off from work. If the work does not involve too much physical activity, you may be able to return sooner.
Total weight loss in the short term after bypass surgery is usually greater than after gastric banding and somewhat better than sleeve gastrectomy.
Vertical Sleeve Gastrectomy (Gastric Sleeve)
In the gastric sleeve surgery, a large portion of the stomach is removed. The new, smaller stomach is about the size of a banana. It limits the amount of food you can eat by making you feel full after eating only small amounts. The procedure can be performed with tiny incisions in the abdomen and a camera for viewing. Operating time and complications may be lower with laparoscopic sleeve gastrectomy compared to bypass procedures.
Most people can go home 2 days after the surgery. You should be able to drink clear liquids on the day after surgery, and eat a puréed diet by the time you go home.
The final weight loss may be close but generally is not quite as large as with gastric bypass. However, it may be enough for many people. Long-term reporting of outcomes from well-designed studies is still considered lacking however. Consult with your doctor about which procedure is best for you.
Weight will usually come off more slowly after gastric sleeve surgery than after gastric bypass. People who have gastric sleeve surgery should keep losing weight for up to 2 to 3 years.
Side Effects and Complications
Risks common to all weight-loss surgeries are:
- Gallstones and gallbladder attacks. These occur from rapid weight loss.
- Gastritis (inflamed stomach lining), heartburn, or stomach ulcers.
- Depression.
- Injury to your stomach, intestines, or other organs during surgery.
- Poor nutrition. You will eat less food after surgery, and your body will not absorb all the calories, protein, vitamins, and minerals from the food you eat.
- Scarring. This could lead to a bowel obstruction (blockage) in the future.
- Vomiting. From eating more than the stomach pouch can hold.
These problems with a gastric band or access port may occur:
- The gastric band may slip partly out of place.
- The gastric band may erode into the wall of the stomach.
- The band may cause heartburn or reflux symptoms.
- The port or tubing may break or leak. Fixing this problem requires a minor procedure.
These problems may occur after gastric bypass:
- A leak can occur from any of the staple lines or from where the intestine is reconnected. If a leak occurs, you will most likely need surgery to repair the leak. The risk of a leak is about 1%.
- The opening between the stomach pouch and your small intestine may get narrower. This is called a stricture. This can be treated by placing a scope down your throat and using a balloon to stretch the opening. Surgery is rarely needed to fix this problem.
- Open surgery may lead to an incisional hernia. Bulging of tissue through the incision.
- Anemia may occur from low iron or vitamin B12 levels.
- Dumping syndrome. This is when the stomach contents move through the small intestine quickly, causing discomfort.
- Kidney stones.
- Thinning of the bones (osteoporosis). May occur due to the body absorbing less vitamin D and calcium.
- People who do not eat enough protein after surgery can become malnourished.
After vertical sleeve gastrectomy, stomach contents may leak from the area where the remaining parts of the stomach are stapled together. You may need another operation to repair this problem if it occurs.
Care after Bariatric Procedures
Most people stay in the hospital for a few days after gastric bypass surgery. You will be discharged when you can:
- Eat liquid or pureed food without vomiting
- Move without too much discomfort
- No longer need pain medication given by injection
You will continue to eat a liquid or soft diet for several weeks after the surgery. After a pouch procedure, the pouch eventually expands to hold about 1 cup (250 mL) of chewed food (a normal stomach can about 1 quart or 1 liter).
Follow-up appointments are essential to determine if you need nutritional supplements such as iron, calcium, or vitamin B12. Supplements, such as a multivitamin with minerals, may be prescribed.
Eat small meals (usually six) throughout the day, rather than large meals that the stomach can no longer handle.
The new stomach probably won't be able to handle both solid food and fluids at the same time. Separate fluid and food intake by at least 30 minutes and only sip what you are drinking.
After surgery, you will have less tolerance of fat, alcohol, and sugar. Reduce your fat intake, especially:
- Deep-fried foods
- Fast-food meals
- High-fat foods
- High-sugar foods, such as cakes, cookies, and candy
Exercise and the support of others (for example, joining a support group with people who have undergone weight-loss surgery) are extremely important to achieving and maintaining weight loss after bariatric surgery.
You can usually start exercising 6 weeks after the operation. Even sooner than that, you should be able to take short walks at a comfortable pace, after consulting with your doctor.
Resources
- 2015-2020 Dietary Guidelines for Americans -- health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines
- American Dietetic Association -- www.eatright.org
- Nutrition.gov -- www.nutrition.gov
- American Society for Bariatric Surgery -- asmbs.org
- Center for Nutrition Policy and Promotion -- www.fns.usda.gov/cnpp
- Food and Nutrition Information Center -- www.nal.usda.gov/fnic
- American Heart Association -- www.heart.org
- National Eating Disorders Organization -- www.nationaleatingdisorders.org/
- Food and Drug Administration -- www.fda.gov
- Weight-Control Information Network -- www.niddk.nih.gov/health-information/community-health-outreach/information-clearinghouses
References
American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Obesity Expert Panel, 2013. Executive summary: guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on practice guidelines. Based on a systematic review from The Obesity Expert Panel, 2013. Obesity (Silver Spring). 2014;22 Suppl 2:S5-S39. PMID: 24961825 www.ncbi.nlm.nih.gov/pubmed/24961825.
American Diabetes Association. Standards of medical care in diabetes - 2019. Diabetes Care. 2019;421(Suppl.1):S13-S28. care.diabetesjournals.org/content/diacare/42/Supplement_1/S13.full.pdf.
Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med. 2015;163(6):437-451. PMID: 26167912 www.ncbi.nlm.nih.gov/pubmed/26167912.
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944-953. PMID: 30389323 www.ncbi.nlm.nih.gov/pubmed/30389323.
Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387(10031):1947-56. PMID: 26868660 www.ncbi.nlm.nih.gov/pubmed/26868660.
Bray GA. Obesity. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 10th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 7.
Centers for Disease Control and Prevention website. Overweight and obesity. www.cdc.gov/obesity. Updated September 12, 2019. Accessed October 28, 2019.
Centers for Disease Control and Prevention website. Tips for parents -- ideas to help children maintain a healthy weight. www.cdc.gov/healthyweight/children/index.html. Updated May 23, 2018. Accessed October 28, 2019.
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8(8):CD003641. PMID: 25105982 www.ncbi.nlm.nih.gov/pubmed/25105982.
Ding SA, McKenzie T, Vernon AH, Goldfine AB. Bariatric surgery. In: Jameson JL, De Groot LJ, de Kretser DM, et al, eds. Endocrinology: Adult and Pediatric. 7th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 27.
Fitzpatrick SL, Wischenka D, Appelhans BM; COMMITTEE ON NUTRITION; COMMITTEE ON ADOLESCENCE; SECTION ON OBESITY., et al. An evidence-based guide for obesity treatment in primary care. Am J Med. 2016;129(1):115.e1-e7. PMID: 26239092 www.ncbi.nlm.nih.gov/pubmed/26239092.
Golden NH, Schneider M, Wood C, et al. Preventing obesity and eating disorders in adolescents. Pediatrics. 2016;138(3). PMID: 27550979 www.ncbi.nlm.nih.gov/pubmed/27550979.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254-266. PMID: 28099824 www.ncbi.nlm.nih.gov/pubmed/28099824.
Jensen MD. Obesity. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 207.
Mancini JG, Filion KB, Atallah R, Eisenberg MJ. Systematic review of the Mediterranean Diet for long-term weight loss. Am J Med. 2016;129(4):407.e4-415.e4. PMID: 26721635 www.ncbi.nlm.nih.gov/pubmed/26721635.
Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev. 2016;11:CD012436. PMID: 27899001 www.ncbi.nlm.nih.gov/pubmed/27899001.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337-372. PMID: 23529351 www.ncbi.nlm.nih.gov/pubmed/23529351.
Millen BE, Wolongevicz DM, Nonas CA, Lichtenstein AH. 2013 American Heart Association/American College of Cardiology/the Obesity Society Guideline for the management of overweight and obesity in adults: implications and new opportunities for registered dietitian nutritionists. J Acad Nutr Diet. 2014;114(11):1730-1735. PMID: 25439081 www.ncbi.nlm.nih.gov/pubmed/25439081.
Moyer VA; U.S. Preventive Services Task Force. Screening for and management of obesity in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(5):373-378. PMID: 22733087 www.ncbi.nlm.nih.gov/pubmed/22733087.
Moyer VA; U.S. Preventive Services Task Force. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2013;132(5):907-914. PMID: 24101758 www.ncbi.nlm.nih.gov/pubmed/24101758.
Oh TJ. The role of anti-obesity medication in prevention of diabetes and its complications. J Obes Metab Syndr. 2019;28(3):158-166. PMID: 31583380 www.ncbi.nlm.nih.gov/pubmed/31583380.
Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882-901. PMID: 30077361 www.ncbi.nlm.nih.gov/pubmed/30077361.
Ryan DH, Kahan S. Guideline Rrecommendations for Oobesity Mmanagement. Med Clin North Am. 2018;102(1):49-63. PMID: 29156187 www.ncbi.nlm.nih.gov/pubmed/29156187.
Semlitsch T, Jeitler K, Berghold A, et al. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database Syst Rev. 2016;3:CD008274. PMID: 26934541 www.ncbi.nlm.nih.gov/pubmed/26934541.
Semlitsch T, Stigler FL, Jeitler K, Horvath K, Siebenhofer A. Management of overweight and obesity in primary care-A systematic overview of international evidence-based guidelines. Obes Rev. 2019;20(9):1218-1230. PMID: 31286668 www.ncbi.nlm.nih.gov/pubmed/31286668.
Sherf Dagan S, Goldenshluger A, Globus I, et al. Nutritional recommendations for adult bariatric surgery patients: clinical practice. Adv Nutr. 2017;8(2):382-394. PMID: 28298280 www.ncbi.nlm.nih.gov/pubmed/28298280.
US Department of Agriculture, Center for Nutrition Policy and Promotion. Dietary Guidelines for Americans, 2015-2020. 8th ed. health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf. Accessed April 10, 2020.
US Food and Drug Administration website. Weight loss drugs. www.fda.gov/drugs/information-drug-class/weight-loss-drugs. Updated December 3, 2015. Accessed June 8, 2023.
US Preventive Services Task Force, Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125(2):361-367. PMID: 20083515 www.ncbi.nlm.nih.gov/pubmed/20083515.
Review Date: 11/10/2019
Reviewed By: David C. Dugdale, III, MD, Professor of Medicine, Division of General Medicine, Department of Medicine, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.