Atrial fibrillation - discharge
Auricular fibrillation - discharge; A-fib - discharge; AF - discharge; Afib - dischargeAtrial fibrillation (Afib) or flutter is a common type of abnormal heartbeat. The heart rhythm is fast and irregular. You were in the hospital to treat this condition.
When You're in the Hospital
You may have been in the hospital because you have Afib. This condition occurs when your heart beats irregularly and often faster than normal. You may have developed this problem while you were in the hospital for a heart attack, heart surgery, or other serious illness such as pneumonia or injury.
Afib
Atrial fibrillation (AFib) and atrial flutter are common types of abnormal heart rhythms (arrhythmias) which affect the upper chambers (atria) of the...
Heart attack
Most heart attacks are caused by a blood clot that blocks one of the coronary arteries. The coronary arteries bring blood and oxygen to the heart. ...

Pneumonia
Pneumonia is inflamed or swollen lung tissue due to infection with a germ. This article covers community-acquired pneumonia (CAP). This type of pneu...

Treatments you may have received include:
- Pacemaker
- Cardioversion (this is a procedure done to change the beat of your heart back to normal. It can be done with medicine or an electric shock.)
- Cardiac ablation
You may have been given medicines to change your heartbeat or slow it down. Some are:
- Beta blockers, such as metoprolol (Lopressor, Toprol-XL) or atenolol (Tenormin)
- Calcium channel blockers, such as diltiazem (Cardizem, Tiazac) or verapamil (Calan, Verelan)
- Digoxin
- Antiarrhythmics (medicines that control heart rhythm), such as amiodarone (Pacerone), flecainide, or sotalol (Betapace)
Taking Your Medicines
Have all of your prescriptions filled before you go home. You should take your medicines the way your health care provider has told you to.
- Tell your provider about other medicines you are taking including over-the-counter medicines, herbs, or supplements. Ask if it is OK to keep taking these. Also, tell your provider if you are taking antacids.
- Never stop taking any of your medicines without first talking to your provider. Do not skip a dose unless you are told to.
- Sometimes certain medicines are prescribed to be taken only when you have symptoms. Be sure you understand when to take your medicines.
You may be taking aspirin or clopidogrel (Plavix), prasugrel (Effient), ticagrelor (Brilinta), warfarin (Coumadin), heparin, or another blood thinner such as apixiban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa) to help keep your blood from clotting.
If you are taking any blood thinner:
- You need to watch for any bleeding or bruising, and let your provider know if it happens.
- Tell your dentist, pharmacist, and other providers that you are taking this medicine.
- You will need to have extra blood tests to make sure your dose is correct if you are taking warfarin.
Lifestyle
Limit how much alcohol you drink. Ask your provider when it is OK to drink, and how much is safe.
Do not smoke cigarettes. If you do smoke, your provider can help you quit.
Follow a heart healthy diet.
- Avoid salty and fatty foods.
- Stay away from fast-food restaurants.
- Your provider can refer you to a dietitian, who can help you plan a healthy diet.
- If you take warfarin, do not make big changes in your diet or take vitamins without checking with your provider.
Try to avoid stressful situations.
- Tell your provider if you feel stressed or sad.
- Talking to a counselor may help.
Learn how to check your pulse, and check it every day.
- It is better to take your own pulse than to use a machine.
- A machine may be less accurate because of atrial fibrillation.
Limit the amount of caffeine you drink (found in coffee, tea, colas, and many other beverages.)
Do not use cocaine, amphetamines, or any other illegal drugs. They may make your heart beat faster, and cause permanent damage to your heart.
Ask your provider for recommendations for physical activity and exercise.
When to Call the Doctor
Call for emergency help if you feel:
- Pain, pressure, tightness, or heaviness in your chest, arm, neck, or jaw
- Shortness of breath
- Gas pains or indigestion
- Sweaty, or if you lose color
- Lightheaded
- Fast heartbeat, irregular heartbeat, or your heart is pounding uncomfortably
- Numbness or weakness in your face, arm, or leg
- Blurry or decreased vision
- Problems speaking or understanding speech
- Dizziness, loss of balance, or falling
- Severe headache
- Bleeding
References
Calkins H, Tomaselli GF, Morady F. Atrial fibrillation: clinical features, mechanisms, and management. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 66.
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2024;149(1):e1-e156. PMID: 38033089 pubmed.ncbi.nlm.nih.gov/38033089/.
Zimetbaum P, Goldman L. Supraventricular ectopy and tachyarrhythmias. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 52.
-
Pacemaker - illustration
A pacemaker is a small, battery-operated electronic device which is inserted under the skin to help the heart beat regularly and at an appropriate rate. The pacemaker has leads that travel through a large vein to the heart, where the wires are anchored. The leads send the electrical impulses to the heart to tell it to beat.
Pacemaker
illustration
-
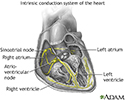
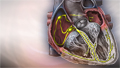
Conduction system of the heart - illustration
The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate the heart to contract.
Conduction system of the heart
illustration
-
How to take your wrist pulse - illustration
How to take your pulse. 1. Place the tips of your index and middle finger on the inside of your wrist below the base of your thumb. 2. Press lightly. You will feel the blood pulsing beneath your fingers. 3. Use a watch or clock with a second hand. Count the beats you feel for 1 minute. Or count the beats for 30 seconds and multiply by 2. This is also called your pulse rate.
How to take your wrist pulse
illustration
-
Pacemaker - illustration
A pacemaker is a small, battery-operated electronic device which is inserted under the skin to help the heart beat regularly and at an appropriate rate. The pacemaker has leads that travel through a large vein to the heart, where the wires are anchored. The leads send the electrical impulses to the heart to tell it to beat.
Pacemaker
illustration
-
Conduction system of the heart - illustration
The intrinsic conduction system sets the basic rhythm of the beating heart by generating impulses which stimulate the heart to contract.
Conduction system of the heart
illustration
-
How to take your wrist pulse - illustration
How to take your pulse. 1. Place the tips of your index and middle finger on the inside of your wrist below the base of your thumb. 2. Press lightly. You will feel the blood pulsing beneath your fingers. 3. Use a watch or clock with a second hand. Count the beats you feel for 1 minute. Or count the beats for 30 seconds and multiply by 2. This is also called your pulse rate.
How to take your wrist pulse
illustration
Review Date: 1/1/2025
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.