Ankylosing spondylitis
Spondylitis; Spondyloarthritis; HLA - B27Ankylosing spondylitis (AS) is a chronic form of arthritis. It mostly affects the bones and joints at the base of the spine where it connects with the pelvis. These joints can become swollen and inflamed. Over time, the affected spinal bones may join together.
Causes
AS is the main member of a family of similar forms of arthritis called spondyloarthritis. Other members include psoriatic arthritis, arthritis of inflammatory bowel disease and reactive arthritis. This family of arthritis affects up to 1 in 100 people.
The cause of AS is unknown, however genes seem to play a role. The majority of people with AS are positive for the HLA-B27 gene, but not everyone who has this gene has AS.
HLA-B27
HLA-B27 is a blood test to look for a protein that is found on the surface of white blood cells. The protein is called human leukocyte antigen B27 (...

The disease often begins between ages 20 and 40, but it may begin before age 10. It affects more males than females.
Symptoms
AS starts with lower back pain that comes and goes but usually becomes present most of the time as the condition progresses.
- Pain and stiffness are worse at night, in the morning, or when you are less active. The discomfort may wake you from sleep.
- The pain often gets better with activity or exercise.
- Back pain may begin in the joint between the pelvis and spine (sacroiliac joints). Over time, it may involve all or part of the spine.
- Your lower spine may become less flexible. Over time, you may stand in a hunched forward position.
Other parts of your body that may be affected include:
- The joints of the shoulders, knees and ankles, which may be swollen and painful
- The joints between your ribs and breastbone, so that you cannot expand your chest fully
- The eye, which may have swelling and redness called uveitis
Fatigue is also a common symptom.
Less common symptoms include:
- Slight fever
AS may occur with other conditions, such as:
-
Psoriasis
Psoriasis
Psoriasis is a skin condition that causes skin redness, silvery scales, and irritation. Most people with psoriasis have thick, red, well-defined pat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Ulcerative colitis or Crohn disease
Crohn disease
Crohn disease is a disease where parts of the digestive tract become inflamed. It most often involves the lower end of the small intestine and the be...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Recurring or chronic eye inflammation (iritis, uveitis)
Eye inflammation
Uveitis is swelling and inflammation of the uvea. The uvea is the middle layer of the wall of the eye. The uvea supplies blood for the iris at the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleIritis
Uveitis is swelling and inflammation of the uvea. The uvea is the middle layer of the wall of the eye. The uvea supplies blood for the iris at the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleUveitis
Uveitis is swelling and inflammation of the uvea. The uvea is the middle layer of the wall of the eye. The uvea supplies blood for the iris at the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Tests may include:
- Anti-cyclic citrullinated peptide (CCP) antibody (which should be negative)
-
Complete blood count (CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - CRP (C reactive protein, a measure of inflammation)
-
ESR (erythrocyte sedimentation rate, a measure of inflammation)
Erythrocyte sedimentation rate
ESR stands for erythrocyte sedimentation rate. It is commonly called a "sed rate. "It is a test that indirectly measures the level of certain protei...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
HLA-B27 antigen (which detects the gene linked to ankylosing spondylitis)
HLA-B27 antigen
HLA-B27 is a blood test to look for a protein that is found on the surface of white blood cells. The protein is called human leukocyte antigen B27 (...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Rheumatoid factor (which should be negative)
-
X-rays of the spine and pelvis
X-rays of the spine and pelvis
A lumbosacral spine x-ray is a picture of the bones (vertebrae) in the lower part of the spine. This area includes the lumbar region and the sacrum,...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
MRI of the spine and pelvis
MRI of the spine and pelvis
A lumbar magnetic resonance imaging (MRI) scan uses energy from strong magnets to create pictures of the lower part of the spine (lumbar spine). An M...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Your health care provider may prescribe medicines such as non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling and pain.
- Some NSAIDs can be bought over-the-counter (OTC). These include aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve, Naprosyn).
- Other NSAIDs are prescribed by your provider.
- Talk to your provider or pharmacist before daily long-term use of any over-the-counter NSAID.
You may also need stronger medicines to control pain and swelling, such as:
- Corticosteroid therapy (such as prednisone) used for short periods of time
- Sulfasalazine
- A biologic tumor necrosis factor (TNF) inhibitor (such as etanercept, adalimumab, infliximab, certolizumab or golimumab)
- A biologic inhibitor of interleukin (IL)17A, secukinumab or Ixekizumab
- Janus kinase (JAK) inhibitors such as tofacitinib and rinvoq
Surgery, such as hip replacement, may be done if pain or joint damage is severe.
Exercises can help improve posture and breathing. Lying flat on your back at night can help you keep a normal posture.
Outlook (Prognosis)
The course of the disease is hard to predict. Over time, signs and symptoms of AS flareup (relapse) and quiet down (remit). Most people are able to function well unless they have a lot of damage to the hips or the spine. Joining a support group of others with the same problem may often help.
Treatment with NSAIDs often reduces the pain and swelling. Treatments given by IV or injection such as TNF inhibitors early in the disease appears to slow progression of the spine arthritis. Other newer medicines such as Interleukin-17 inhibitors and oral medicines, JAK inhibitors may help people if other medicines have not worked well.
Rarely, people with ankylosing spondylitis may have problems with:
- Psoriasis, a chronic skin disorder
- Inflammation in the eye (uveitis)
- Inflammation in the intestine (colitis)
Colitis
Colitis is swelling (inflammation) of the large intestine (colon).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Abnormal heart rhythm
- Scarring or thickening of the lung tissue
- Scarring or thickening of the aortic heart valve
- Spinal cord injury after a fall
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of ankylosing spondylitis
- You have ankylosing spondylitis and develop new symptoms during treatment
References
Inman RD, Fitzgerald G. Classification and epidemiology of spondyloarthritis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 75.
Inman RD, Rahman P. Spondyloarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 244.
Taylor WJ, van der Linden SJEF, Robinson PC, Brown M, Østergaard M, Gensler LS. Axial spondyloarthritis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 76.
Ward MM, Deodhar A, Gensler LS, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Care Res (Hoboken). 2019;71(10):1285-1299. PMID: 31436026 pubmed.ncbi.nlm.nih.gov/31436026/.
-
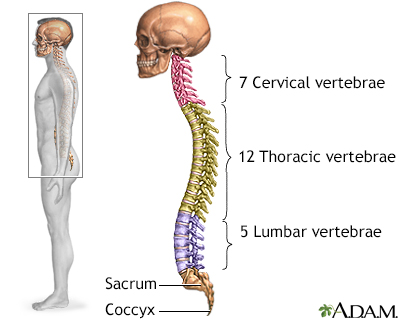
Skeletal spine - illustration
The spine is divided into several sections. The cervical vertebrae make up the neck. The thoracic vertebrae comprise the chest section and have ribs attached. The lumbar vertebrae are the remaining vertebrae below the last thoracic bone and the top of the sacrum. The sacral vertebrae are caged within the bones of the pelvis, and the coccyx represents the terminal vertebrae or vestigial tail.
Skeletal spine
illustration
-
Cervical spondylosis - illustration
Cervical spondylosis is a disorder that results from abnormal growth of the bones of the neck and degeneration and mineral deposits in the cushions between the vertebrae. Progressive neck pain is a key indication of cervical spondylosis. It may be the only symptom in many cases. Examination often shows limited ability to bend the head toward the shoulders and limited ability to rotate the head. The goal of treatment is relief of pain and prevention of permanent spinal cord and nerve root injury.
Cervical spondylosis
illustration
-
Skeletal spine - illustration
The spine is divided into several sections. The cervical vertebrae make up the neck. The thoracic vertebrae comprise the chest section and have ribs attached. The lumbar vertebrae are the remaining vertebrae below the last thoracic bone and the top of the sacrum. The sacral vertebrae are caged within the bones of the pelvis, and the coccyx represents the terminal vertebrae or vestigial tail.
Skeletal spine
illustration
-
Cervical spondylosis - illustration
Cervical spondylosis is a disorder that results from abnormal growth of the bones of the neck and degeneration and mineral deposits in the cushions between the vertebrae. Progressive neck pain is a key indication of cervical spondylosis. It may be the only symptom in many cases. Examination often shows limited ability to bend the head toward the shoulders and limited ability to rotate the head. The goal of treatment is relief of pain and prevention of permanent spinal cord and nerve root injury.
Cervical spondylosis
illustration
Review Date: 4/1/2025
Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.