Osteoarthritis
Hypertrophic osteoarthritis; Osteoarthrosis; Degenerative joint disease; DJD; OA; Arthritis - osteoarthritisOsteoarthritis (OA) is the most common joint disorder. It is due to aging and wear and tear on a joint.
Causes
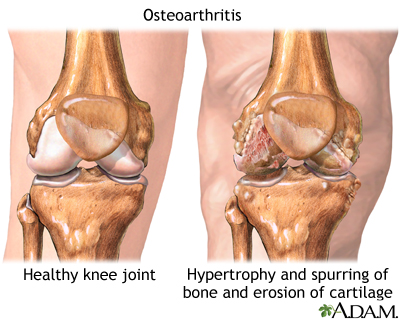
Cartilage is the firm, rubbery tissue that cushions your bones at the joints. It allows bones to glide over one another when the joint moves. When the cartilage breaks down and wears away, the fragments of the cartilage or the bones rub together. This often causes the pain, swelling, and stiffness of OA.
As OA worsens, bony spurs or extra bone may form around the joint. The ligaments and muscles around the joint may become weaker and stiffer.
Before age 55, OA occurs equally in men and women. After age 55, it is more common in women.
Other factors can also lead to OA.
- OA tends to run in families.
- Being overweight increases the risk for OA in the hip, knee, ankle, and foot joints. This is because extra weight causes more wear and tear.
- Fractures or other joint injuries can lead to OA later in life. This includes injuries to the cartilage and ligaments in your joints.
- Jobs that involve kneeling or squatting for more than an hour a day, or involve lifting, climbing stairs, or walking increase the risk for OA.
- Playing sports that involve direct impact on the joint (football), twisting (basketball or soccer), or throwing also increase the risk for OA.
Medical conditions that can lead to OA or symptoms similar to OA include:
- Bleeding disorders that cause bleeding in the joint, such as hemophilia
Hemophilia
Hemophilia refers to a group of bleeding disorders in which blood clotting takes a longer time than normal. There are two forms of hemophilia:Hemophi...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Disorders that block the blood supply near a joint and lead to bone death (avascular necrosis)
Avascular necrosis
Osteonecrosis is bone death caused by poor blood supply. It is most common in the hip and shoulder but can affect other large joints such as the kne...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Other types of arthritis, such as long-term (chronic) gout, pseudogout, or rheumatoid arthritis
Gout
Gout is a type of arthritis. It occurs when uric acid builds up in the blood and causes inflammation in the joints. Acute gout is a painful conditio...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticlePseudogout
Calcium pyrophosphate dihydrate (CPPD) arthritis is a joint disease that can cause attacks of arthritis. Like gout, crystals form in the joints. Bu...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleRheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Symptoms of OA often appear in middle age. Almost everyone has some symptoms of OA by age 70.
Pain and stiffness in the joints are the most common symptoms. The pain is often worse:
- After exercise
- When you put weight or pressure on the joint
- When you use the joint
With OA, your joints may become stiffer and harder to move over time. You may notice a rubbing, grating, or crackling sound when you move the joint.
Morning stiffness refers to the pain and stiffness you feel when you first wake up in the morning. Stiffness due to OA often lasts for 30 minutes or less. It can last more than 30 minutes if there is inflammation in the joint. It often improves after activity, allowing the joint to warm up.
During the day, the pain may get worse when you are active and feel better when you are resting. As OA gets worse, you may have pain even when you are resting. And it may wake you up at night.
Some people might not have symptoms, even though x-rays show the physical changes of OA.
Exams and Tests
Your health care provider will examine you and ask about your symptoms. The exam may show:
- Joint movement that causes a crackling (grating) sound, called crepitation
- Joint swelling (either due to fluid in the joint or the bones around the joints feeling larger than normal)
- Limited range of motion
- Tenderness when the joint is pressed
- Normal movement is often painful
Blood tests are not helpful in diagnosing OA. They can be used to look for alternative conditions, such as rheumatoid arthritis or gout.
An x-ray will likely show:
- Loss of the joint space
- Wearing down of the ends of the bone
- Bone spurs
- Bony changes near the joint, called subchondral cysts
Treatment
OA cannot be cured, but OA symptoms can be controlled. OA will most likely get worse over time though the pace with which this occurs varies from person to person.
You can have surgery, but other treatments can improve your pain and make your life much better. Although these treatments cannot make the OA go away, they can often delay surgery or make your symptoms mild enough to not cause significant problems.
MEDICINES
Over-the-counter (OTC) pain relievers, such as acetaminophen (Tylenol) or a nonsteroidal anti-inflammatory drug (NSAID) can help with OA symptoms. You can buy these medicines without a prescription.
Over-the-counter (OTC) pain relievers
Over-the-counter (OTC) pain relievers can help relieve pain or lower a fever. Over-the-counter means you can buy these medicines without a prescript...

It is recommended that you should not take more than 3 grams (3,000 milligrams) of acetaminophen a day. If you have liver disease, talk with your provider before taking acetaminophen. Over the counter NSAIDs include aspirin, ibuprofen, and naproxen. Several other NSAIDs are available by prescription. Talk with your provider before taking an NSAID on a regular basis.
Duloxetine (Cymbalta) is a prescription medicine that can also help treat long-term (chronic) pain related to OA.
Chronic
Chronic refers to something that continues over an extended period of time. A chronic condition is usually long-lasting and does not easily or quick...

Injections of steroid medicines into the arthritic joint often provide significant short to medium-term benefits from the pain of OA.
Injections
The pain, swelling, and stiffness of arthritis can limit your movement. Medicines can help manage your symptoms so that you can continue to lead an ...

Other medicines that may help include:
- Pills, such as glucosamine and chondroitin sulfate
- Capsaicin skin cream to relieve pain
LIFESTYLE CHANGES
Staying active and getting exercise can maintain joint and overall movement. Ask your provider to recommend an exercise routine or refer you to a physical therapist. Water exercises, such as swimming, are often helpful.
Other lifestyle tips include:
- Applying heat or cold to the joint
- Eating healthy foods
- Getting enough rest
- Losing weight if you are overweight
- Protecting your joints from injury
If the pain from OA gets worse, keeping up with activities may become more difficult or painful. Making changes around the home can help take stress off your joints to relieve some of the pain. If your work is causing stress in certain joints, you may need to adjust your work area or change work tasks.
PHYSICAL THERAPY
Physical therapy can help improve muscle strength and the motion of stiff joints as well as your balance. If therapy does not make you feel better after 6 to 12 weeks, then it likely will not be helpful.
Massage therapy may provide short-term pain relief but does not change the underlying OA process. Make sure you work with a licensed massage therapist who is experienced in working on sensitive joints.
BRACES
Splints and braces may help support weakened joints. Some types limit or prevent the joint from moving. Others may shift pressure off one portion of a joint. Use a brace only when your provider or therapist recommends one. Using a brace the wrong way can cause joint damage, stiffness, and pain.
ALTERNATIVE TREATMENTS
Acupuncture is a traditional Chinese treatment. It is thought that when acupuncture needles stimulate certain points on the body, chemicals that block pain are released. Acupuncture may provide significant pain relief for OA.
Yoga and Tai chi have also shown significant benefit in treating the pain from OA.
S-adenosylmethionine (SAMe, pronounced Sammy) is a manmade form of a natural chemical in the body. It may help reduce joint inflammation and pain.
SURGERY
Severe cases of OA might benefit from surgery to replace or repair damaged joints. Options include:
- Arthroscopic surgery to trim torn and damaged cartilage
- Changing the alignment of a bone to relieve stress on the bone or joint (osteotomy)
- Surgical fusion of bones, often in the spine (arthrodesis)
Arthrodesis
Spinal fusion is surgery to permanently join together two or more bones in the spine so there is no movement between them. These bones are called ve...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Total or partial replacement of the damaged joint with an artificial joint (knee replacement, hip replacement, shoulder replacement, ankle replacement, and elbow replacement)
Knee replacement
Knee joint replacement is a surgery to replace a knee joint with a man-made artificial joint. The artificial joint is called a prosthesis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHip replacement
Hip joint replacement is surgery to replace all or part of the hip joint with a man-made joint. The artificial joint is called a prosthesis....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleShoulder replacement
Shoulder replacement is surgery to replace the bones of the shoulder joint with artificial joint parts.
Read Article Now Book Mark ArticleAnkle replacement
Ankle replacement is surgery to replace the damaged bone and cartilage in the ankle joint. Artificial joint parts (prosthetics) are used to replace ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleElbow replacement
Elbow replacement is surgery to replace the elbow joint with artificial joint parts (prosthetics).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Support Groups
Organizations that specialize in arthritis are good resources for more information on OA.
Information on OA
The following organizations provide more information on arthritis:American Academy of Orthopaedic Surgeons -- orthoinfo. aaos. org/en/diseases--condi...

Outlook (Prognosis)
Your movement may become limited over time. Doing everyday activities, such as personal hygiene, household chores, or cooking may become a challenge. Treatment usually improves function.
When to Contact a Medical Professional
Contact your provider if you have symptoms of OA that are bothersome or get worse.
Prevention
Try not to overuse a painful joint at work or during activities. Maintain a normal body weight. Keep the muscles around your joints strong, especially the weight-bearing joints (knee, hip, or ankle).
References
Hunter DJ. Osteoarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 241.
Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2020;72(2):149-162. PMID: 31908149 pubmed.ncbi.nlm.nih.gov/31908149/.
Misra D, Kumar D, Neogi T. Treatment of osteoarthritis. In: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 106.
-
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
Osteoarthritis - illustration
Osteoarthritis is associated with the aging process and can affect any joint. The cartilage of the affected joint is gradually worn down, eventually causing bone to rub against bone. Bony spurs develop on the unprotected bones causing pain and inflammation.
Osteoarthritis
illustration
-
Arthroscopy - illustration
Knee arthroscopy is surgery that is done to check for problems, using a tiny camera to see inside your knee. Other medical instruments may also be inserted to repair your knee.
Arthroscopy
illustration
-
Knee misaligned due to arthritis - illustration
Arthritis of the knee is a result of wearing away of the cartilage within the knee joint. Normally, cartilage protects a joint and allows it to move smoothly. When cartilage breaks down and wears away, the bones in the knee rub together, causing pain, swelling, and stiffness. Over time, the breakdown of tissues within the joint can cause the bones in the knee to move out of their normal position or become misaligned. The joint may angle inward (knock-kneed) or angle outward (bow-legged).
Knee misaligned due to arthritis
illustration
-
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
Osteoarthritis - illustration
Osteoarthritis is associated with the aging process and can affect any joint. The cartilage of the affected joint is gradually worn down, eventually causing bone to rub against bone. Bony spurs develop on the unprotected bones causing pain and inflammation.
Osteoarthritis
illustration
-
Arthroscopy - illustration
Knee arthroscopy is surgery that is done to check for problems, using a tiny camera to see inside your knee. Other medical instruments may also be inserted to repair your knee.
Arthroscopy
illustration
-
Knee misaligned due to arthritis - illustration
Arthritis of the knee is a result of wearing away of the cartilage within the knee joint. Normally, cartilage protects a joint and allows it to move smoothly. When cartilage breaks down and wears away, the bones in the knee rub together, causing pain, swelling, and stiffness. Over time, the breakdown of tissues within the joint can cause the bones in the knee to move out of their normal position or become misaligned. The joint may angle inward (knock-kneed) or angle outward (bow-legged).
Knee misaligned due to arthritis
illustration
Review Date: 5/20/2024
Reviewed By: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.