Testicular torsion
Torsion of the testis; Testicular ischemia; Testicular twistingTesticular torsion is twisting of the spermatic cord, which supports the testes in the scrotum. When this occurs, the blood supply is cut off to the testicles and nearby tissue in the scrotum. This may cause permanent damage to the testicle.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...

Causes
Some men are more prone to this condition because of defects in the connective tissue within the scrotum. The problem may also occur after an injury to the scrotum that results in a lot of swelling, or following heavy exercise. In some cases, there is no clear cause.
The condition is more common during the first year of life and at the beginning of adolescence (puberty). However, it may happen in older men.
Symptoms
Symptoms include:
- Sudden severe pain in one testicle. The pain may occur without a clear reason.
- Swelling within one side of the scrotum (scrotal swelling).
Scrotal swelling
Scrotal swelling is abnormal enlargement of the scrotum. This is the name for the sac surrounding the testicles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nausea or vomiting.
Nausea or vomiting
Nausea is feeling an urge to vomit. It is often called "being sick to your stomach. "Vomiting or throwing-up forces the contents of the stomach up t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Additional symptoms that may be associated with this disease:
-
Testicle lump
Testicle lump
A testicle lump is swelling or a growth (mass) in one or both testicles.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Blood in the semen
Blood in the semen
Blood in the semen is called hematospermia. It may be in amounts too small to be seen except with a microscope, or it may be visible in the ejaculat...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Testicle pulled to a higher position in scrotum than normal (high riding)
Exams and Tests
Your health care provider will examine you. The exam may show:
- Extreme tenderness and swelling in the testicle area.
- The testicle on the affected side is higher.
You may have a Doppler ultrasound of the testicle to check the blood flow. There will be no blood flowing through the area if you have complete torsion. Blood flow may be reduced if the spermatic cord is only partly twisted.
Treatment
Most of the time, surgery is needed to correct the problem. The procedure involves untwisting the cord and sewing the testicle to the inside wall of the scrotum. Surgery should be done as soon as possible after symptoms begin. If it is performed within 6 hours, most of the testicle can be saved.
During surgery, the testicle on the other side is often secured into place as well. This is because the unaffected testicle is at risk of testicular torsion in the future.
Outlook (Prognosis)
The testicle may continue to function properly if the condition is found early and treated right away. The chances that the testicle will need to be removed increase if blood flow is reduced for more than 6 hours. However, sometimes it may lose its ability to function even if torsion has lasted fewer than 6 hours.
Possible Complications
The testicle may shrink if its blood supply is cut off for an extended time. It may need to be surgically removed. Shrinkage of the testicle may occur days to months after the torsion has been corrected. Severe infection of the testicle and scrotum is also possible if the blood flow is limited for a long period.
When to Contact a Medical Professional
Get emergency medical attention if you have symptoms of testicular torsion as soon as possible. It is better to go to an emergency room instead of an urgent care in case you need to have surgery right away.
Prevention
Take steps to avoid injury to the scrotum. Many cases cannot be prevented.
References
Di Carlo HN, Crigger CB. Disorders and anomalies of the scrotal contents. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 582.
Germann CA. Urologic disorders. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 85.
Palmer LS, Palmer JS. Management of abnormalities of the external genitalia in males. In: Domochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 55.
Park JH, Leitner DV, Elsamra SE. Evaluation of the urologic patient: history and physical examination. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 2.
Zee RS, Herndon CDA. Perinatal urology. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 34.
-
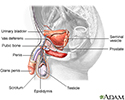
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
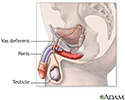
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Testicular torsion repair - series
Presentation
-
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Testicular torsion repair - series
Presentation
Review Date: 7/1/2025
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.