Epilepsy
Seizure disorder; Epileptic - epilepsyEpilepsy is a brain disorder in which a person has repeated seizures over time. Seizures are episodes of uncontrolled and abnormal electrical activity of brain cells that may cause changes in attention or behavior, such as bodily movements.
Seizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...

Causes
Epilepsy occurs when changes in the brain cause it to be too excitable or irritable. As a result, the brain cells send out abnormal electrical signals. This leads to repeated, unpredictable seizures. (A single seizure that does not happen again is not epilepsy.)
Epilepsy may be due to a medical condition or injury that affects the brain. Or, the cause may be unknown (idiopathic).
Common causes of epilepsy include:
-
Stroke or transient ischemic attack (TIA)
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleTransient ischemic attack
A transient ischemic attack (TIA) occurs when blood flow to a part of the brain stops for a brief time. A person will have stroke-like symptoms for ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Dementia, such as Alzheimer disease
Dementia
Dementia is a loss of brain function that occurs with certain diseases. It affects one or more brain functions such as memory, thinking, language, j...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleAlzheimer disease
Dementia is a loss of brain function that occurs with certain diseases. Alzheimer disease (AD) is the most common form of dementia. It affects memo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Traumatic brain injury
Traumatic brain injury
A traumatic brain injury (TBI) can occur when the head hits an object, or a moving object strikes the head. There are three types of TBI:Mild TBI, a...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infections, including brain abscess, meningitis, encephalitis, and HIV/AIDS
Brain abscess
A brain abscess is a collection of pus, immune cells, and other material in the brain, caused by a bacterial or fungal infection.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMeningitis
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEncephalitis
Encephalitis is irritation and swelling (inflammation) of the brain, most often due to infections.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHIV/AIDS
Human immunodeficiency virus (HIV) is the virus that causes acquired immunodeficiency syndrome (AIDS). When a person becomes infected with HIV, the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Brain problems that are present at birth (congenital brain defect)
- Brain injury that occurs during or near birth
- Metabolism disorders present at birth (such as phenylketonuria)
Phenylketonuria
Phenylketonuria (PKU) is a rare condition in which a baby is born without the ability to properly break down an amino acid called phenylalanine....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Brain tumor
- Abnormal blood vessels in the brain
- Other illness that damages or destroys brain tissue
- Seizure disorders that run in families (hereditary epilepsy)
Epileptic seizures can happen to anyone at any age. However, they're more common in young children and people age 65 years and older. There may be a family history of seizures or epilepsy.
Symptoms
Symptoms vary from person to person. Some people may have simple staring spells. Others have violent shaking and loss of alertness (convulsion). The type of seizure depends on the part of the brain that is affected.
Most of the time, for people with epilepsy, their seizures are similar to ones before it. Some people with epilepsy have a strange sensation before each seizure. Sensations may be tingling, smelling an odor that is not actually there, or emotional changes. This is called an aura.
Your health care provider can tell you more about the specific type of seizure you may have:
-
Absence seizures (also called non-motor seizures) include seizures involving a change in behavior but without changes in motor movement (such as staring spells). They may occur along with generalized seizures.
Absence seizures
An absence seizure is the term for a type of seizure involving staring spells. This type of seizure is a brief (usually less than 15 seconds) change...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Focal onset seizures may occur with no change in awareness. Symptoms depend on what part of the brain is affected. These seizures may spread to the whole brain.
Focal onset seizures
All seizures are caused by abnormal electrical disturbances in the brain. Focal seizures occur when this electrical activity is in a limited area of...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Generalized seizures involve both sides of the brain and cause impaired awareness. Abnormal movements involving the whole body are often present. Clenching of the jaw and losing control of the urine or bowels may occur.
Generalized seizures
Bilateral tonic-clonic seizure is a type of seizure that involves the entire body. It is also called grand mal seizure. The terms generalized seizu...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your provider will perform a physical exam. This will include a detailed look at brain and nervous system function.
An electroencephalogram (EEG) will be done to check the electrical activity in the brain. People with epilepsy often have abnormal electrical activity seen on this test. In some cases, the test shows the area in the brain where the seizures start. The brain's electrical activity may appear normal after a seizure or between seizures.
Electroencephalogram
An electroencephalogram (EEG) is a test to measure the electrical activity of the brain.

Tests that may be done include:
- Blood chemistry
-
Blood sugar
Blood sugar
A blood sugar test measures the amount of sugar (glucose) in a sample of your blood. Glucose is a major source of energy for most cells of the body, ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Complete blood count (CBC)
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Kidney function tests
Kidney function tests
Kidney function tests are common lab tests used to evaluate how well the kidneys are working. Such tests include:BUN (Blood urea nitrogen) Creatinin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Genetic tests
-
Liver function tests
Liver function tests
Liver function tests are common tests that are used to see how well the liver is working. Tests include:AlbuminAlpha-1 antitrypsinAlkaline phosphata...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lumbar puncture (spinal tap)
Lumbar puncture
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Tests for infectious diseases
Head CT or MRI scan is often done to find the cause and location of the problem in the brain.
CT
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.

MRI
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...

To diagnose epilepsy or plan for epilepsy surgery, you may also need to:
- Wear an EEG recorder for days or weeks as you go about your everyday life.
- Stay in a special hospital where brain activity can be recorded while video cameras capture what happens to you during the seizure. This is called a video EEG.
Treatment
Treatment for epilepsy includes taking medicines, lifestyle changes, and sometimes surgery.
If epilepsy is due to a tumor, abnormal blood vessels, or bleeding in the brain, surgery to treat these disorders may make the seizures stop.
Medicines to prevent seizures, called antiseizure medicines (also called anticonvulsants or antiepileptic medicines), may reduce the number of future seizures:
- These medicines are taken by mouth. Which type you are prescribed depends on the type of seizures you have.
- Your dosage may need to be changed from time to time. You may need regular blood tests to check for side effects.
- Always take your medicine on time and as directed. Missing a dose can cause you to have a seizure. Do not stop taking or change medicines on your own. Talk to your provider first.
- Many epilepsy medicines cause birth defects. Women who plan to become pregnant should tell their provider in advance in order to adjust medicines.
Many epilepsy medicines may affect the health of your bones. Talk to your provider about whether you need vitamins and other supplements.
Epilepsy that does not get better after 2 or 3 anti-seizure medicines have been tried is called medically refractory epilepsy. In this case, your provider may recommend surgery to:
- Remove the abnormal brain cells causing the seizures.
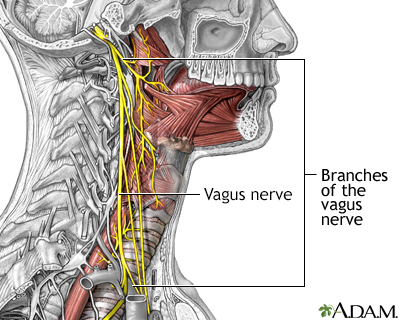
- Place a vagal nerve stimulator (VNS). This device is similar to a heart pacemaker. It can help reduce the number of seizures.
Some children are placed on a special diet to help prevent seizures. The most popular one is the ketogenic diet. A diet low in carbohydrates, such as the Atkins diet, may also be helpful in some adults. Be sure to discuss these options with your provider before trying them.
Lifestyle or medical changes can increase the risk for a seizure in adults and children with epilepsy. Talk with your provider about:
Adults
You have epilepsy. People with epilepsy have seizures. A seizure is a sudden brief change in the electrical and chemical activity in the brain. Aft...
Children
Your child has epilepsy. People with epilepsy have seizures. A seizure is a sudden brief change in the electrical and chemical activity in the brai...

- New prescribed medicines, vitamins, or supplements
- Emotional stress
- Illness, especially infection
- Lack of sleep
- Pregnancy
- Skipping doses of epilepsy medicines
- Use of alcohol or other recreational drugs
- Exposure to flickering lights or stimuli
- Hyperventilation
Other considerations:
- People with epilepsy should wear medical alert jewelry so that prompt treatment can be obtained if a seizure occurs.
- People with poorly controlled epilepsy should not drive. Check your state's law about which people with a history of seizures are allowed to drive.
- Do not use machinery or do activities that require constant awareness, such as climbing to high places, biking, and swimming alone. Having a seizure during these activities can result in serious injury and death.
Support Groups
The stress of having epilepsy or being a caretaker of someone with epilepsy can often be helped by joining a support group. In these groups, members share common experiences and problems.
Support group
The following organizations are good resources for information on epilepsy:Centers for Disease Control and Prevention -- www. cdc. gov/epilepsy/index...

Outlook (Prognosis)
Some people with epilepsy may be able to reduce or even stop their anti-seizure medicines after having no seizures for several years. Certain types of childhood epilepsy go away or improve with age, usually in the late teens or 20s.
For many people, epilepsy is a lifelong condition. In these cases, anti-seizure medicines need to be continued. There is a very low risk for sudden death with epilepsy.
Possible Complications
Complications may include:
- Difficulty learning
- Breathing in food or saliva into the lungs during a seizure, which can cause aspiration pneumonia
Aspiration pneumonia
Pneumonia is inflammation (swelling) and infection of the lungs or large airways. Aspiration pneumonia occurs when food or liquid is breathed into th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injury from falls, bumps, self-inflicted bites, driving or operating machinery during a seizure
- Permanent brain damage (stroke or other damage)
- Side effects of medicines
When to Contact a Medical Professional
Call 911 or the local emergency number if:
- This is the first time a person has a seizure.
- A seizure occurs in someone who is not wearing a medical ID bracelet (which has instructions explaining what to do).
In the case of someone who has had seizures before, call 911 or the local emergency number for any of these emergency situations:
- This is a longer seizure than the person normally has, or an unusual number of seizures for the person.
- Repeated seizures over a few minutes.
- Repeated seizures in which consciousness or normal behavior is not regained between them (status epilepticus).
Contact your provider if any new symptoms occur:
- Loss of hair
- Nausea or vomiting
- Rash
- Side effects of medicines, such as drowsiness, restlessness, confusion, sedation
- Tremors or abnormal movements, or problems with coordination
Prevention
There is no known way to prevent epilepsy. Proper diet and sleep, and staying away from alcohol and illegal drugs may decrease the likelihood of triggering seizures in people with epilepsy.
You can reduce your risk for a head injury by wearing a helmet during risky activities. This can lessen the likelihood of a brain injury that leads to seizures and epilepsy.
References
Abou-Khalil BW, Gallagher MJ, Macdonald RL. Epilepsies. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 100.
Epilepsy Foundation website. Facts & statistics about epilepsy. www.epilepsy.com/what-is-epilepsy/statistics. Updated February 27, 2019. Accessed April 28, 2025.
Epilepsy Foundation website. Who can get epilepsy? www.epilepsy.com/what-is-epilepsy/understanding-seizures/who-gets-epilepsy. Updated February 4, 2022. Accessed April 28, 2025.
Wiebe S. The epilepsies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 372.
-
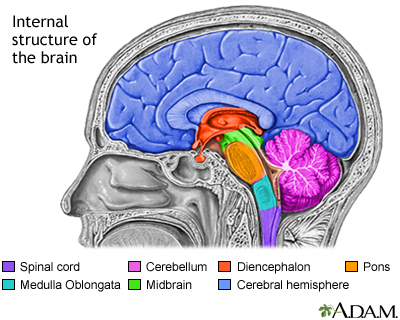
Brain structures - illustration
The structures of the brain include the brainstem, consisting of the spinal cord, the medulla oblongata, the pons and the midbrain; the cerebellum; the cerebrum (one half, or hemisphere shown), and the diencephalon.
Brain structures
illustration
-
Limbic system - illustration
The limbic system of the brain is a group of structures which govern emotions and behavior. The limbic system, and in particular the hippocampus and amygdala, is involved in the formation of long-term memory, and is closely associated with the olfactory structures (having to do with the sense of smell).
Limbic system
illustration
-
Role of the vagus nerve in epilepsy - illustration
The vagus nerves branch off the brain on either side of the head and travel down the neck, along the esophagus to the intestinal tract. They are the longest nerves in the body, and affect swallowing and speech. The vagus nerves also connect to parts of the brain involved in seizures. In many seizures disorders, electrical stimulation of the vagus nerves may afford relief of symptoms.
Role of the vagus nerve in epilepsy
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system is made up of the brain and the spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
-
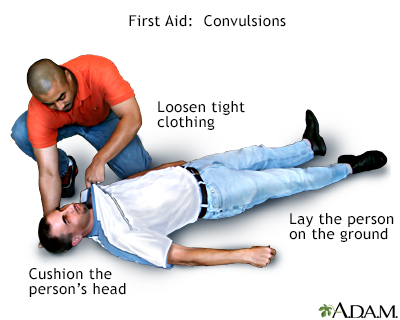
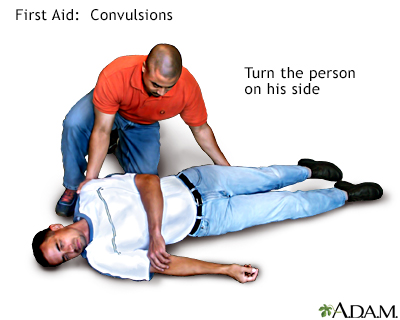
Convulsions - first aid - series
Presentation
-
Brain structures - illustration
The structures of the brain include the brainstem, consisting of the spinal cord, the medulla oblongata, the pons and the midbrain; the cerebellum; the cerebrum (one half, or hemisphere shown), and the diencephalon.
Brain structures
illustration
-
Limbic system - illustration
The limbic system of the brain is a group of structures which govern emotions and behavior. The limbic system, and in particular the hippocampus and amygdala, is involved in the formation of long-term memory, and is closely associated with the olfactory structures (having to do with the sense of smell).
Limbic system
illustration
-
Role of the vagus nerve in epilepsy - illustration
The vagus nerves branch off the brain on either side of the head and travel down the neck, along the esophagus to the intestinal tract. They are the longest nerves in the body, and affect swallowing and speech. The vagus nerves also connect to parts of the brain involved in seizures. In many seizures disorders, electrical stimulation of the vagus nerves may afford relief of symptoms.
Role of the vagus nerve in epilepsy
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system is made up of the brain and the spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
-
Convulsions - first aid - series
Presentation
Review Date: 4/16/2025
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.