Cerebral palsy
Spastic paralysis; Paralysis - spastic; Spastic hemiplegia; Spastic diplegia; Spastic quadriplegiaCerebral palsy (CP) is a group of disorders that involve the brain. This affects nervous system functions, such as movement, learning, hearing, seeing, and thinking.
There are several different types of CP, including spastic, dyskinetic, ataxic, hypotonic, and mixed.
Causes
CP is caused by injuries or abnormalities of the brain. Most of these problems occur as the baby grows in the womb. But they can happen at any time during the first 2 years of life, while the baby's brain is still developing.
In some people with cerebral palsy, parts of the brain are injured due to a low level of oxygen (hypoxia) in those areas. It is not known why this occurs.
Hypoxia
Cerebral hypoxia occurs when there is not enough oxygen getting to the brain. The brain needs a constant supply of oxygen and nutrients to function....
Premature infants have a slightly higher risk of developing CP. It may also occur in early infancy as a result of certain conditions such as:
- Bleeding in the brain
- Brain infections (encephalitis, meningitis, herpes simplex infections)
Encephalitis
Encephalitis is irritation and swelling (inflammation) of the brain, most often due to infections.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMeningitis
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Head injury
Head injury
A head injury is any trauma to the scalp, skull, or brain. Head injury can be either closed or open (penetrating). A closed head injury means you rec...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infections in the mother during pregnancy (rubella)
Rubella
Rubella, also known as the German measles, is an infection in which there is a rash on the skin. Congenital rubella is when a pregnant woman with rub...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Untreated jaundice
Jaundice
Newborn jaundice occurs when a baby has a high level of bilirubin in the blood. Bilirubin is a yellow substance that the body creates when it replac...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injuries to the brain during the childbirth process
- Exposure to toxins (such as mercury) while developing
In some cases, the cause of CP is never determined.
Symptoms
Symptoms of CP can be very different between people with this group of disorders. Symptoms may:
- Be very mild or very severe
- Only involve one side of the body or both sides
- Be more pronounced in either the arms or legs, or involve both the arms and legs
Symptoms are usually seen before a child is 2 years old. Sometimes symptoms begin as early as 3 months. Parents may notice that their child is delayed in reaching developmental stages such as sitting, rolling, crawling, or walking.
There are several different types of cerebral palsy. Some people have a mix of symptoms.
Spastic CP is the most common type. Symptoms include:
- Muscles that are very tight and do not stretch. They may tighten even more over time.
- Abnormal walk (gait) -- arms tucked in toward the sides, knees crossed or touching, legs make "scissor" movements, walk on the toes.
- Joints are tight and do not open all the way (called joint contracture).
- Muscle weakness or loss of movement in a group of muscles (paralysis).
Paralysis
Muscle function loss is when a muscle does not work or move normally. The medical term for complete loss of muscle function is paralysis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Symptoms may affect one arm or leg, one side of the body, both legs, or both arms and legs.
The following symptoms may occur in other types of CP:
- Abnormal movements (twisting, jerking, or writhing) of the hands, feet, arms, or legs while awake, which gets worse during periods of stress
-
Tremors
Tremors
A tremor is a type of shaking movement. A tremor is most often noticed in the hands and arms. It may affect any body part, including the head, tong...
Read Article Now Book Mark Article - Unsteady gait
-
Loss of coordination
Loss of coordination
Uncoordinated movement is due to a muscle control problem that causes an inability to coordinate movements. It leads to a jerky, unsteady, to-and-fr...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Floppy muscles, especially at rest, and joints that move around too much
Other brain and nervous system symptoms may include:
- Learning disabilities are common, but intelligence can be normal
- Speech problems (dysarthria)
Dysarthria
Dysarthria is a condition in which you have difficulty saying words because of problems with the muscles that help you talk.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hearing or vision problems
Vision problems
There are many types of eye problems and vision disturbances, such as: Halos Blurred vision (the loss of sharpness of vision and the inability to see...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Seizures
Seizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pain, especially in adults, which can be difficult to manage
Eating and digestion symptoms:
- Difficulty sucking or feeding in infants, or chewing and swallowing in older children and adults
- Vomiting or constipation
Other symptoms:
- Increased drooling
- Slower than normal growth
-
Irregular breathing
Irregular breathing
An arrhythmia is a disorder of the heart rate (pulse) or heart rhythm. The heart can beat too fast (tachycardia), too slow (bradycardia), or irregul...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Urinary incontinence
Urinary incontinence
Urinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider will perform a full neurologic exam. In older people, testing cognitive function is also important.
Other tests may be performed as needed, most often to check for other disorders:
- Blood tests
-
CT scan of the head
CT scan of the head
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cranial ultrasound (especially in pre-term infants)
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Electroencephalogram (EEG)
EEG
An electroencephalogram (EEG) is a test to measure the electrical activity of the brain.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hearing screen
-
MRI of the head
MRI of the head
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Vision testing
Treatment
There is no cure for CP. The goal of treatment is to help the person be as independent as possible.
Treatment requires a team approach, including:
- Primary care provider
- Dentist (dental check-ups are recommended around every 6 months)
- Social worker
- Nurses
- Occupational, physical, and speech therapists
- Other specialists, including a neurologist, rehabilitation physician (physiatrist), pulmonologist, and gastroenterologist
Treatment is based on the person's symptoms and the need to prevent complications.
Self and home care include:
- Getting enough food and nutrition
- Keeping the home safe
- Performing exercises recommended by the providers
- Practicing proper bowel care (stool softeners, fluids, fiber, laxatives, regular bowel habits)
- Protecting the joints from injury
Putting the child in regular schools is recommended unless physical disabilities or mental development makes this impossible. Special education or schooling may help.
The following may help with communication and learning:
- Glasses
- Hearing aids
- Muscle and bone braces
- Walking aids
- Wheelchairs
Physical therapy, occupational therapy, orthopedic help, or other treatments may also be needed to help with daily activities and care.
Medicines may include:
- Anticonvulsants to prevent or reduce the frequency of seizures
- Botulinum toxin to help with spasticity and drooling
- Muscle relaxants to reduce tremors and spasticity
Surgery may be needed in some cases to:
- Control gastroesophageal reflux
Gastroesophageal reflux
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). F...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Cut certain nerves from the spinal cord to help with pain and spasticity
- Place a pump for medicine administration into spinal canal
- Place a feeding tube
- Release joint contractures
Shockwave therapy to reduce spasticity is being investigated.
Support Groups
Stress and burnout among parents and other caregivers of people with cerebral palsy is common. Seek support and more information from organizations that specialize in CP.
Organizations that specialize in CP
The following organizations are good resources for information on cerebral palsy:Centers for Disease Control and Prevention -- www. cdc. gov/cerebral...

Outlook (Prognosis)
CP is a life-long disorder. Long-term care may be required. The disorder does not affect expected length of life. The amount of disability varies. Babies with mild CP may outgrow their symptoms.
Many adults are able to live in the community, either independently or with different levels of help.
Possible Complications
CP may lead to the following health problems:
- Bone thinning (osteoporosis)
Osteoporosis
Osteoporosis is a disease in which bones become fragile and more likely to break (fracture).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bowel obstruction
Bowel obstruction
Intestinal obstruction is a partial or complete blockage of the bowel. The contents of the intestine cannot pass through it.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Hip dislocation and arthritis in the hip joint
Dislocation
A dislocation is a disruption of the normal position of the ends of two or more bones where they meet at a joint. A joint is the place where two bon...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleArthritis
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injuries from falls
-
Pressure sores
Pressure sores
A pressure sore is an area of the skin that breaks down when something keeps rubbing or pressing against the skin.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Joint contractures
-
Pneumonia caused by choking
Pneumonia
Pneumonia is inflamed or swollen lung tissue due to infection with a germ. This article covers community-acquired pneumonia (CAP). This type of pneu...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Poor nutrition
- Reduced communication skills (sometimes)
- Reduced intellect (sometimes)
-
Scoliosis
Scoliosis
Scoliosis is an abnormal curving of the spine. Your spine is your backbone. It runs straight down your back. Everyone's spine naturally curves a b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Seizures (in about half of the people who are affected by cerebral palsy)
- Social stigma
When to Contact a Medical Professional
Contact your provider if symptoms of CP develop, especially if you know that an injury occurred during birth or early infancy.
Prevention
Getting the proper prenatal care may reduce the risk for some rare causes of CP. In most cases though, the injury causing the disorder is not preventable.
Pregnant mothers with certain medical conditions may need to be followed in a high-risk prenatal clinic.
Adults with CP should continue to follow-up with a neurologist to reduce the risk of late complications.
References
Barkoudah E. Encephalopathies. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 638.
Barkoudah E, Srivastava S, deGusmao C, Coulter D. Cerebral palsy. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 111.
Greenberg JM, Narendran V, Brady JM, Nathan AT, Haberman BB. Neonatal morbidities of prenatal and perinatal origin. In: Lockwood CJ, Copel JA, Dugoff L, et al, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2023:chap 73.
Otero-Luis I, Martinez-Rodrigo A, Cavero-Redondo I, et al. Efficacy of selective dorsal rhizotomy in the treatment of spasticity in children with cerebral palsy: a systematic review and meta-analysis. J Neurosurg Pediatr. 2025;35(6):571-580. PMID: 40117662 pubmed.ncbi.nlm.nih.gov/40117662/.
Smith SE, Gannotti M, Hurvitz EA, et al. Adults with cerebral palsy require ongoing neurologic care: a systematic review. Ann Neurol. 2021;89(5):860-871. PMID: 33550625 pubmed.ncbi.nlm.nih.gov/33550625/.
-
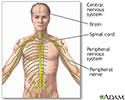
Central nervous system and peripheral nervous system - illustration
The central nervous system is made up of the brain and the spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
Review Date: 7/17/2025
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.