Allergies
Allergy - allergies; Allergy - allergensAn allergy is an immune response or reaction to substances that are usually not harmful.
Immune response
The immune response is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful....

Causes
Allergies are very common. Both genes and environment play a role. If both your parents have allergies, there is a good chance that you could also have allergies.
The immune system normally protects the body against harmful substances, such as bacteria and viruses. The immune system can also react to foreign substances called allergens. These allergens are usually harmless, and in most people do not cause a problem.
Allergens
An allergen is a substance that can cause an allergic reaction. In some people, the immune system recognizes allergens as foreign or dangerous. As ...

In a person with allergies, the immune response is oversensitive. When it recognizes an allergen, the immune system launches a response. Chemicals such as histamines are released. These chemicals cause allergy symptoms.
Common allergens include:
- Drugs
- Dust
- Food
-
Insect venom
Insect venom
Insect bites and stings can cause an immediate skin reaction. The bite from fire ants and the sting from bees, wasps, and hornets are most often pai...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Mold
- Pet and other animal dander
- Pollen
Some people have allergy-like reactions to hot or cold temperatures, sunlight, or other environmental triggers. Sometimes, friction (rubbing or roughly stroking the skin) will cause symptoms.
Allergies may make certain medical conditions, such as sinus problems, eczema, and asthma, worse.
Eczema
Atopic dermatitis is a long-term (chronic) skin disorder that involves scaly and itchy rashes. It is a type of eczema. Other forms of dermatitis inc...

Asthma
Asthma is a chronic disease that causes the airways of the lungs to swell and become narrow. It leads to breathing difficulty such as wheezing, shor...

Symptoms
Mostly, the part of the body the allergen touches determines what symptoms you develop. For example:
-
Allergens that you breathe in often cause a stuffy nose, itchy nose and throat, mucus, cough, and wheezing.
Allergens that you breathe in
Allergic rhinitis is a diagnosis associated with a group of symptoms affecting the nose. These symptoms occur when you breathe in something you are ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleWheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Allergens that touch the eyes may cause itchy, watery, red, swollen eyes.
Allergens that touch the eyes
The conjunctiva is a clear layer of tissue lining the eyelids and covering the white of the eye. Allergic conjunctivitis occurs when the conjunctiva...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Allergens that touch the skin can cause a skin rash, hives, itching, blisters, or skin peeling.
Skin rash
Contact dermatitis is a condition in which the skin becomes red, sore, or inflamed after direct contact with a substance.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHives
Hives are raised, usually itchy, red bumps (welts) on the surface of the skin. They can be an allergic reaction to food or medicine. They can also ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Medicine allergies and food allergies may involve the whole body and can lead to a variety of symptoms.
Medicine allergies
Drug allergies are a group of symptoms caused by an allergic reaction to a drug (medicine).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
At times, an allergy can trigger a response that involves the entire body.
Exams and Tests
The health care provider will perform a physical exam and ask questions, such as when the allergy symptoms occur.
Allergy testing may be needed to find out whether the symptoms are an actual allergy or are caused by other problems. For example, eating contaminated food (food poisoning) may cause symptoms similar to food allergies. Some medicines (such as aspirin and ampicillin) can produce non-allergic reactions, including rashes. A runny nose or cough may actually be due to an infection.
Food poisoning
Food poisoning occurs when you swallow food or water that contains bacteria, parasites, viruses, or the toxins made by these germs. Most cases are c...

Skin testing is the most common method of allergy testing:
Skin testing
Allergy skin tests are used to find out which substances cause a person to have an allergic reaction. These substances are called allergens....

- The prick test involves placing a small amount of the suspected allergy-causing substances on the skin, and then slightly pricking the area so the substance goes under the skin. The skin is closely watched for signs of a reaction, which include swelling and redness.
- The intradermal test involves injecting a tiny amount of allergen under your skin, then watching the skin for a reaction.
- Both the prick and intradermal tests are read 15 minutes after application of the test.
- The patch test involves placing a patch with the suspected allergen on your skin. The skin is then closely watched for signs of a reaction. This test is used to determine contact allergy. It is usually read 48 to 72 hours after application of the test.
The provider may also check your reaction to physical triggers by applying heat, cold, or other stimulation to your body and watching for an allergic response.
Blood tests that may be done include:
- Immunoglobulin E (IgE), which measures levels of allergy-related substances
-
Complete blood count (CBC) during which an eosinophil white blood cell count is done
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEosinophil white blood cell count
An absolute eosinophil count is a blood test that measures the number of one type of white blood cells called eosinophils. Eosinophils become active...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
In some cases, the provider may tell you to avoid certain items to see if you get better, or to use suspected items to see if you feel worse. This is called "use or elimination testing." This is often used to check for food or medicine allergies.
Treatment
Severe allergic reactions (anaphylaxis) need to be treated with a medicine called epinephrine. It can be life-saving when given right away. If you use epinephrine, call 911 or the local emergency number and go straight to the hospital.
Anaphylaxis
Anaphylaxis is a life-threatening type of allergic reaction.

The best way to reduce symptoms is to avoid what causes your allergies. This is especially important for food and medicine allergies.
There are several types of medicines to prevent and treat allergies. Which medicine your provider recommends depends on the type and severity of your symptoms, your age, and overall health.
Illnesses that are caused by allergies (such as asthma, hay fever, and eczema) may need other treatments.
Medicines that can be used to treat allergies include:
ANTIHISTAMINES
Antihistamines are available over-the-counter and by prescription. They are available in many forms, including:
- Capsules and pills
- Eye drops
- Injection
- Liquid
- Nasal spray
CORTICOSTEROIDS
These are anti-inflammatory medicines. They are available in many forms, including:
- Creams, lotions, and ointment for the skin
- Eye drops
-
Nasal spray
Nasal spray
A nasal corticosteroid spray is a medicine to help make breathing through the nose easier.
Read Article Now Book Mark Article - Lung inhaler
- Pills
- Injection
People with severe allergic symptoms may be prescribed corticosteroid pills or injections for short periods.
DECONGESTANTS
Decongestants help relieve a stuffy nose. Do not use decongestant nasal spray for more than several days because they can cause a rebound effect and make the congestion worse. Decongestants in pill form do not cause this problem. People with high blood pressure, heart problems, or prostate enlargement should use decongestants with caution.
OTHER MEDICINES
Leukotriene inhibitors are medicines that block the substances that trigger allergies. People with asthma and indoor and outdoor allergies may be prescribed these medicines.
ALLERGY SHOTS
Allergy shots (immunotherapy) are sometimes recommended if you cannot avoid the allergen and your symptoms are hard to control. Allergy shots keep your body from over-reacting to the allergen. You will get regular injections of the allergen. Each dose is slightly larger than the last dose until a maximum dose is reached. Allergy shots are only used for environmental allergies (pollens, pet dander, dust) or venom allergies. These shots do not work for everybody and you will have to visit the provider often.
Immunotherapy
An allergy shot is a medicine that is injected into your body to treat allergy symptoms.
SUBLINGUAL IMMUNOTHERAPY TREATMENT (SLIT)
Instead of shots, medicine put under the tongue may help for grass, ragweed, and dust mite allergies.
ORAL IMMUNOTHERAPY (OIT)
For people with peanut allergy, oral immunotherapy may be an option. This treatment involves eating tiny amounts of peanut powder and slowly increasing the dose over time until they are eating the equivalent of about 1 peanut every day. OIT is a treatment rather than a cure of food allergy and there is a risk of allergic reaction with the dosing of the peanut powder. This requires a significant commitment of time for visits to the provider and dosing at home.
XOLAIR:
Xolair (omalizumab) is a medication that was recently approved for the treatment of food allergies. Xolair does not cure food allergies but can decrease a person’s likelihood of reacting to a tiny amount of their food allergen. Xolair is an injection that is given either once a month or every 2 weeks, depending on the results of a blood test. People can be allergic to Xolair and there may be an increased risk of certain cancers or heart issues in people taking Xolair. Talk to your provider about Xolair if you have food allergies.
Support Groups
Ask your provider if there are any asthma and allergy support groups in your area.
Asthma and allergy support groups
The following organizations are good resources for information on asthma and allergies:Allergy and Asthma Network -- allergyasthmanetwork. org/Americ...
Outlook (Prognosis)
Most allergies can be easily treated with medicine.
Some children may outgrow an allergy, especially food allergies. But once a substance has triggered an allergic reaction, it usually continues to affect the person.
Allergy shots are most effective when used to treat hay fever and insect sting allergies. They are not used to treat food allergies because of the danger of a severe reaction.
Allergy shots may need years of treatment, but they work in most cases. However, they may cause uncomfortable side effects (such as hives and rash) and dangerous outcomes (such as anaphylaxis). Talk with your provider whether allergy drops (SLIT) are right for you.
Treatments for food allergies are evolving quickly. Speak with your provider about different food allergy treatments available.
Possible Complications
Complications that may result from allergies or their treatment include:
-
Anaphylaxis (life-threatening allergic reaction)
Anaphylaxis
Anaphylaxis is a life-threatening type of allergic reaction.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Breathing problems and discomfort during the allergic reaction
- Drowsiness and other side effects of medicines
When to Contact a Medical Professional
Contact your provider for an appointment if:
- Severe symptoms of allergy occur
- Treatment for allergies no longer works
Prevention
Breastfeeding may help prevent certain food allergies when you feed babies this way only for 4 to 6 months. However, changing a mother's diet during pregnancy or while breastfeeding does not seem to help prevent allergies.
For most children, changing the diet or using special formulas does not seem to prevent allergies. If a parent, brother, sister, or other family member has a history of eczema and allergies, discuss feeding with your child's doctor. Infants with eczema or food allergy often benefit from early introduction (before 12 months of life) of peanuts and/or eggs. Discuss with your child’s provider if this is something that you should do.
There is also evidence that being exposed to certain allergens (such as dust mites and cat dander) in the first year of life may prevent some allergies. This is called the "hygiene hypothesis." It came from the observation that infants on farms tend to have fewer allergies than those who grow up in more sterile environments. However, older children do not seem to benefit.
Once allergies have developed, treating the allergies and carefully avoiding allergy triggers can prevent reactions in the future.
References
Chiriac AM, Bousquet J, Demoly P. In vivo methods for the study and diagnosis of allergy. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 67.
Custovic A, Tovey E. Allergen control for prevention and management of allergic diseases. In: Burks AW, Holgate ST, O'Hehir RE, et al, eds. Middleton's Allergy: Principles and Practice. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 84.
Nadeau KC. Approach to the patient with allergic or immunologic disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 230.
Wallace DV, Dykewicz MS, Oppenheimer J, Portnoy JM, Lang DM. Pharmacologic treatment of seasonal allergic rhinitis: synopsis of guidance from the 2017 Joint Task Force on Practice Parameters. Ann Intern Med. 2017;167(12):876-881. PMID: 29181536 pubmed.ncbi.nlm.nih.gov/29181536/.
Wise SK, Damask C, Greenhawt M, et al. A synopsis of guidance for allergic rhinitis diagnosis and management from ICAR 2023. J Allerg Clin Immun Pactice. 2023;11(3):773-796.PMID: 36894277. pubmed.ncbi.nlm.nih.gov/36894277/.
-
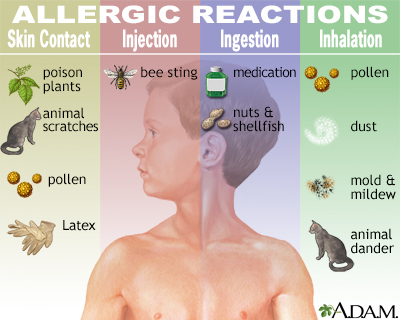
Allergic reactions - illustration
Allergic reaction can be provoked by skin contact with poison plants, chemicals and animal scratches, as well as by insect stings. Ingesting or inhaling substances like pollen, animal dander, molds and mildew, dust, nuts and shellfish, may also cause allergic reaction. Medications such as penicillin and other antibiotics are also to be taken with care, to assure an allergic reflex is not triggered.
Allergic reactions
illustration
-
Allergy symptoms - illustration
The immune system normally responds to harmful substances such as bacteria, viruses and toxins by producing symptoms such as runny nose and congestion, post-nasal drip and sore throat, and itchy ears and eyes. An allergic reaction can produce the same symptoms in response to substances that are generally harmless, like dust, dander or pollen. The sensitized immune system produces antibodies to these allergens, which cause chemicals called histamines to be released into the bloodstream, causing itching, swelling of affected tissues, mucus production, hives, rashes, and other symptoms. Symptoms vary in severity from person to person.
Allergy symptoms
illustration
-
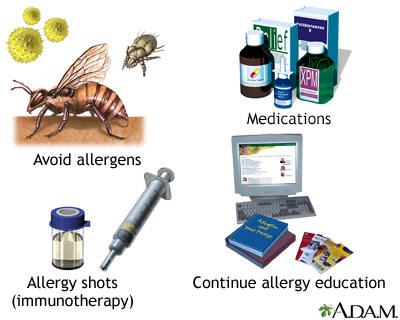
Introduction to allergy treatment - illustration
Treatment varies with the severity and type of allergy symptom. The first course of action is to avoid the allergen if possible. Medications such as antihistamines are then usually prescribed to relieve the allergic symptoms. Immunotherapy, or allergy shots, is occasionally recommended if the allergen cannot be avoided. It includes regular injections of the allergen, given in increasing doses that may de-sensitize the body to the allergen.
Introduction to allergy treatment
illustration
-
Hives (urticaria) on the arm - illustration
Hives (urticaria) are raised, red, itchy welts, seen here on the arm. The majority of urticaria develop as a result of allergic reactions. Occasionally, they may be associated with autoimmune diseases, infections (parasitosis), drugs, malignancy, or other causes.
Hives (urticaria) on the arm
illustration
-
Hives (urticaria) on the chest - illustration
Hives (urticaria) are raised, red, itchy welts, seen here on the chest. The majority of urticaria develop as a result of allergic reactions. Occasionally they may be associated with autoimmune diseases, infections (parasitosis), drugs, malignancy, or other causes.
Hives (urticaria) on the chest
illustration
-
Allergies - illustration
Heredity, environmental conditions, number and type of exposures and emotional factors can indicate a predisposition to allergies.
Allergies
illustration
-
Antibodies - illustration
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Antibodies
illustration
-
Histamine is released - illustration
Mast cells release histamine when an allergen is encountered. The histamine response can produce sneezing, itching, hives and watery eyes.
Histamine is released
illustration
-
Allergic reactions - illustration
Allergic reaction can be provoked by skin contact with poison plants, chemicals and animal scratches, as well as by insect stings. Ingesting or inhaling substances like pollen, animal dander, molds and mildew, dust, nuts and shellfish, may also cause allergic reaction. Medications such as penicillin and other antibiotics are also to be taken with care, to assure an allergic reflex is not triggered.
Allergic reactions
illustration
-
Allergy symptoms - illustration
The immune system normally responds to harmful substances such as bacteria, viruses and toxins by producing symptoms such as runny nose and congestion, post-nasal drip and sore throat, and itchy ears and eyes. An allergic reaction can produce the same symptoms in response to substances that are generally harmless, like dust, dander or pollen. The sensitized immune system produces antibodies to these allergens, which cause chemicals called histamines to be released into the bloodstream, causing itching, swelling of affected tissues, mucus production, hives, rashes, and other symptoms. Symptoms vary in severity from person to person.
Allergy symptoms
illustration
-
Introduction to allergy treatment - illustration
Treatment varies with the severity and type of allergy symptom. The first course of action is to avoid the allergen if possible. Medications such as antihistamines are then usually prescribed to relieve the allergic symptoms. Immunotherapy, or allergy shots, is occasionally recommended if the allergen cannot be avoided. It includes regular injections of the allergen, given in increasing doses that may de-sensitize the body to the allergen.
Introduction to allergy treatment
illustration
-
Hives (urticaria) on the arm - illustration
Hives (urticaria) are raised, red, itchy welts, seen here on the arm. The majority of urticaria develop as a result of allergic reactions. Occasionally, they may be associated with autoimmune diseases, infections (parasitosis), drugs, malignancy, or other causes.
Hives (urticaria) on the arm
illustration
-
Hives (urticaria) on the chest - illustration
Hives (urticaria) are raised, red, itchy welts, seen here on the chest. The majority of urticaria develop as a result of allergic reactions. Occasionally they may be associated with autoimmune diseases, infections (parasitosis), drugs, malignancy, or other causes.
Hives (urticaria) on the chest
illustration
-
Allergies - illustration
Heredity, environmental conditions, number and type of exposures and emotional factors can indicate a predisposition to allergies.
Allergies
illustration
-
Antibodies - illustration
Antigens are large molecules (usually proteins) on the surface of cells, viruses, fungi, bacteria, and some non-living substances such as toxins, chemicals, drugs, and foreign particles. The immune system recognizes antigens and produces antibodies that destroy substances containing antigens.
Antibodies
illustration
-
Histamine is released - illustration
Mast cells release histamine when an allergen is encountered. The histamine response can produce sneezing, itching, hives and watery eyes.
Histamine is released
illustration
Review Date: 3/31/2024
Reviewed By: Deborah Pedersen, MD, MS, Allergy & Asthma Care, PC, Taunton, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.