Undescended testicle
Cryptorchidism; Empty scrotum - undescended testes; Scrotum - empty (undescended testes); Monorchism; Vanished testes - undescended; Retractile testesUndescended testicle occurs when one or both testicles fail to move into the scrotum before birth.
Causes
Most of the time, a boy's testicles descend into the scrotum by the time he is 6 months old. Undescended testicles are common in infants who are born early. The problem occurs less in full-term infants.
Testicles
The testes are 2 egg-shaped male reproductive organs located in the scrotum. They produce sperm and the male hormone, testosterone.

Some babies have a condition called retractile testes and the health care provider may not be able to find the testicles. In this case, the testicle is normal, but is pulled back out of the scrotum by a muscle reflex. This occurs because the testicles are still small before puberty. The testicles will descend normally at puberty and surgery is not needed.
Scrotum
The scrotum is a part of a male's body that is located below the penis. The scrotum is the sac (pouch) that contains the testes, epididymis, and the...

Testicles that do not naturally descend into the scrotum are considered abnormal. An undescended testicle is more likely to develop cancer, even if it is brought into the scrotum with surgery. Cancer is also more likely in the other testicle.
Bringing the testicle into the scrotum can improve sperm production and increase the chances of good fertility. It also allows the provider to do an exam for the early detection of cancer.
In other cases, no testicle may be found, even during surgery. This may be due to a problem that occurred while the baby was still developing before birth.
Symptoms
Most of the time there are no symptoms other than the absence of the testicle in the scrotum. (This is called an empty scrotum.)
Exams and Tests
An exam by the provider confirms that one or both of the testicles are not in the scrotum.
The provider may or may not be able to feel the undescended testicle in the abdominal wall above the scrotum.
Imaging tests, such as an ultrasound or CT scan, may be done.
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.

CT scan
A computed tomography (CT) scan is an imaging method that uses x-rays to create pictures of cross-sections of the body. Related tests include:Abdomin...

Treatment
In most cases, the testicle will descend without treatment during the child's first year. If this does not occur, treatment may include:
- Hormone injections (B-HCG or testosterone) to try to bring the testicle into the scrotum.
-
Surgery (orchiopexy) to bring the testicle into the scrotum. This is the main treatment.
Surgery (orchiopexy)
Undescended testicle repair is surgery to correct testicles that have not dropped down into the correct position in the scrotum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Having surgery early may prevent damage to the testicles and avoid infertility. An undescended testicle that is found later in life may need to be removed. This is because the testicle is not likely to function well and could pose a risk for cancer.
Outlook (Prognosis)
Most of the time, the problem goes away without treatment. Medicine or surgery to correct the condition is successful in most cases. Once the condition is corrected, you should have routine testicle exams by your provider.
In about 50% of males with undescended testicles, the testicles cannot be found at the time of surgery. This is called a vanished or absent testis. As stated earlier, it may be due to something while the baby was still developing during pregnancy.
Possible Complications
Complications may include:
- Damage to the testicle from surgery
- Infertility later in life
-
Testicular cancer in one or both testes
Testicular cancer
Testicular cancer is cancer that starts in the testicles. The testicles are the male reproductive glands located in the scrotum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Contact your child's provider if he appears to have an undescended testicle.
References
Di Carlo HN, Crigger CB. Disorders and anomalies of the scrotal contents. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 582.
Kraft KH. Etiology, diagnosis, and management of the undescended testis. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 57.
Robertson RP. Testicular dysgenesis syndrome and testicular tumors. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 115.
-
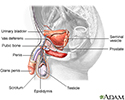
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
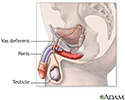
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Before and after testicular repair - illustration
In normal fetal development, during the last months of birth, the testicles develop in the abdomen and descend into the scrotum in the male fetus. Sometimes at birth, one or both testicles may fail to descend into the scrotum. If the testicle has not descended within the first year of the baby's life, surgery may be recommended to return the testicle to its proper position in the scrotum.
Before and after testicular repair
illustration
-
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Before and after testicular repair - illustration
In normal fetal development, during the last months of birth, the testicles develop in the abdomen and descend into the scrotum in the male fetus. Sometimes at birth, one or both testicles may fail to descend into the scrotum. If the testicle has not descended within the first year of the baby's life, surgery may be recommended to return the testicle to its proper position in the scrotum.
Before and after testicular repair
illustration
Review Date: 7/1/2025
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.