Cleft lip and palate
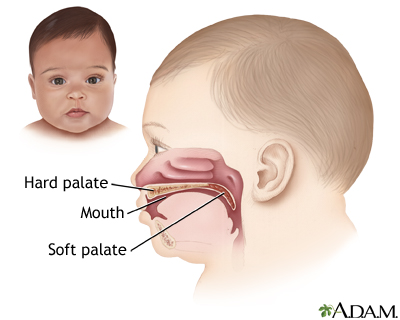
Cleft palate; Craniofacial defectCleft lip and palate are birth defects that affect the upper lip and the roof of the mouth.
Causes
There are many causes of cleft lip and palate. Problems with genes passed down from 1 or both parents, drugs, medicines, viruses, or other toxins can all cause these birth defects. Cleft lip and palate may occur along with other syndromes or birth defects.
A cleft lip and palate can:
- Affect the appearance of the face
- Lead to problems with feeding and speech
- Lead to ear infections
Babies are more likely to be born with a cleft lip and palate if they have a family history of these conditions or other birth defects.
Symptoms
A child may have one or more birth defects and the severity can vary significantly.
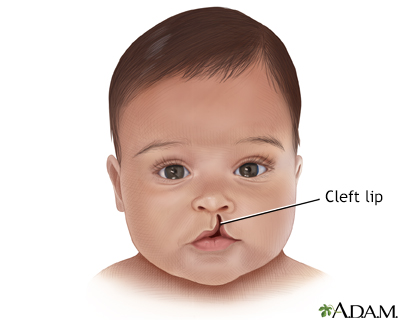
A cleft lip may be just a small notch in the lip. It may also be a complete split in the lip that goes all the way to the base of the nose.
A cleft palate can be on one or both sides of the roof of the mouth. It may go the full length of the palate.
Other symptoms include:
- Change in nose shape (how much the shape changes varies)
- Poorly aligned teeth
Problems that may be present because of a cleft lip or palate are:
- Failure to gain weight
- Feeding problems
- Flow of milk through nasal passages during feeding
-
Poor growth
Poor growth
Delayed growth is poor or abnormally slow height or weight gains in a child younger than age 5. This may just be normal, and the child may outgrow i...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Repeated ear infections
-
Speech difficulties
Speech difficulties
A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can ma...
Read Article Now Book Mark Article
Exams and Tests
A physical exam of the mouth, nose, and palate confirms a cleft lip or cleft palate. Medical tests may be done to rule out other possible health conditions.
Treatment
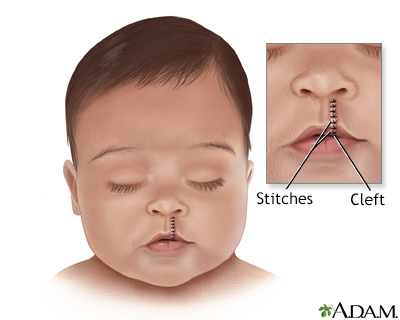
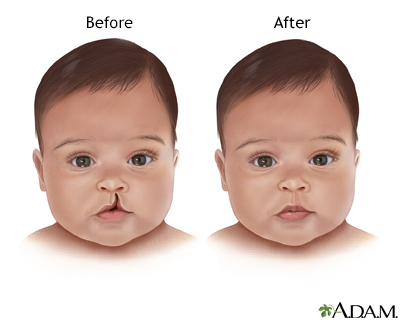
Surgery to close the cleft lip is often done when the child is between 2 to 9 months old. Surgery may be needed later in life if the problem has a major effect on the nose area. Some patients may receive tympanostomy tubes during the surgery also.
Surgery to close the cleft lip
Cleft lip and cleft palate repair is surgery to fix birth defects of the upper lip and palate (roof of the mouth).

A cleft palate is most often closed within the first year of life so that the child's speech develops normally. Sometimes, a prosthetic device is temporarily used to close the palate so the baby can feed and grow until surgery can be done.
Continued follow-up may be needed with speech therapists and orthodontists.
Support Groups
For more resources and information, see cleft palate support groups.
Cleft palate support groups
The following organizations are good resources for information on cleft palate:American Cleft Palate (ACPA) Craniofacial Association -- acpacares. or...

Outlook (Prognosis)
Most babies will heal without problems. How your child will look after healing depends on the severity of their condition. Your child might need another surgery to fix the scar from the surgery wound.
Children who had a cleft palate repair may need to see a dentist or orthodontist. Their teeth may need to be corrected as they come in.
Hearing problems are common in children with cleft lip or palate. Your child should have a hearing test at an early age, and it should be repeated over time.
Your child may still have problems with speech after the surgery. This is caused by muscle problems in the palate. Speech therapy will help your child.
When to Contact a Medical Professional
Cleft lip and palate is most often diagnosed at birth. Follow your health care provider's recommendations for follow-up visits. Contact your provider if problems develop between visits.
References
Dhar VK. Cleft lip and palate. In: Kliegman RM, St. Geme JW, Blum NJ, et al, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 356.
Wang TD, Milczuk HA. Cleft lip and palate. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 188.
Review Date: 4/6/2025
Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.