Acute bronchitis
Acute bronchitis is swelling and inflamed tissue in the bronchi, the main passages that carry air to the lungs. This swelling narrows the airways, which makes it harder to breathe. Other symptoms of bronchitis are a cough and coughing up mucus. Acute means the symptoms have been present only for a short time.
Causes
When acute bronchitis occurs, it almost always comes after having a cold or flu-like illness. The bronchitis infection is usually caused by a virus. At first, it affects your nose, sinuses, and throat. Then it spreads to the airways that lead to your lungs.
Sometimes, bacteria also infect your airways. This is more common in people with chronic obstructive pulmonary disease chronic obstructive pulmonary disease (COPD).
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe. There are two main forms of COPD:Chroni...

Chronic bronchitis is a long-term condition. To be diagnosed with chronic bronchitis, you must have a cough with mucus on most days for at least 3 months.
Symptoms
Some symptoms of acute bronchitis are:
- Chest discomfort
-
Cough that produces mucus -- the mucus may be clear or yellow-green
Cough
Coughing is an important way to keep your throat and airways clear. But too much coughing may mean you have a disease or disorder. Some coughs are d...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fatigue
Fatigue
Fatigue is a feeling of weariness, tiredness, or lack of energy.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Fever -- usually low-grade
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Shortness of breath that gets worse with activity
Shortness of breath
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Wheezing, in people with asthma
Wheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Even after acute bronchitis has cleared, you may have a dry, nagging cough that lasts for 1 to 4 weeks.
Sometimes it can be hard to know if you have pneumonia or bronchitis. If you have pneumonia, you are more likely to have a high fever and chills, feel sicker, or feel more short of breath.
Pneumonia
Pneumonia is inflamed or swollen lung tissue due to infection with a germ. This article covers community-acquired pneumonia (CAP). This type of pneu...

Exams and Tests
Your health care provider will listen to the breathing sounds in your lungs with a stethoscope. Your breathing may sound abnormal or rough.
Tests may include:
-
Chest x-ray, if your provider suspects pneumonia
Chest x-ray
A chest x-ray is an x-ray of the chest, lungs, heart, large arteries, ribs, and diaphragm.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pulse oximetry, a painless test that helps determine the amount of oxygen in your blood by using a device placed on the end of your finger
Treatment
Most people DO NOT need antibiotics for acute bronchitis caused by a virus. The infection will almost always go away on its own within 1 week, though a mild cough may persist for up to 3 weeks. Doing these things may help you feel better:
- Drink plenty of fluids.
- If you have asthma or another chronic lung condition, use your inhaler.
Asthma
Asthma is a chronic disease that causes the airways of the lungs to swell and become narrow. It leads to breathing difficulty such as wheezing, shor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleInhaler
Using a metered-dose inhaler (MDI) seems simple. But many people do not use them the right way. If you use your MDI the wrong way, less medicine ge...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Get plenty of rest.
- Take aspirin or acetaminophen if you have a fever. DO NOT give aspirin to people under age 18.
- Breathe moist air by using a humidifier or steaming up the bathroom.
Humidifier
A home humidifier can increase the humidity (moisture) in your home. This helps eliminate the dry air that can irritate and inflame the airways in y...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Certain medicines that you can buy without a prescription can help break up or loosen mucus. Look for the word "guaifenesin" on the label. If needed, ask the pharmacist for help finding it.
If your symptoms do not improve or if you are wheezing, your provider may prescribe an inhaler to open your airways.
Wheezing
Wheezing is a high-pitched whistling sound during breathing. It occurs when air moves through narrowed breathing tubes in the lungs.

If your provider thinks you also have bacteria in your airways, they may prescribe antibiotics. This medicine will only get rid of bacteria, not viruses.
Your provider may also prescribe corticosteroid medicine to reduce swelling in your lungs.
If you have influenza and it is caught in the first 48 hours after getting sick, your provider might also prescribe antiviral medicine.
Influenza
The flu (influenza) is a viral respiratory illness that causes fever, chills, runny nose, body aches, and cough. It spreads easily from person to pe...

Other tips include:
- DO NOT smoke.
- Avoid secondhand smoke and air pollution.
- Wash your hands (and your children's hands) often to avoid spreading viruses and other germs.
Outlook (Prognosis)
Except for the cough, symptoms usually go away in 7 to 10 days if you do not have a lung disorder. Coughing often lasts for 2 to 3 weeks.
When to Contact a Medical Professional
Contact your provider if you:
- Have a cough on most days, or have a cough that keeps returning
- Are coughing up blood
- Have a high fever or shaking chills
Chills
Chills refers to feeling cold after being in a cold environment. The word can also refer to an episode of shivering along with paleness and feeling ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Have a low-grade fever for 3 or more days
- Have thick, yellow-green mucus, especially if it has a bad smell
- Feel short of breath or have chest pain
- Have a chronic illness, like heart or lung disease
References
Bearman GM, Wenzel RP. Acute bronchitis and tracheitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 84.
Centers for Disease Control and Prevention website. Acute bronchitis. Chest cold (acute bronchitis) basics. www.cdc.gov/acute-bronchitis/about/. Updated April 17, 2024. Accessed June 18, 2024.
Cherry JD. Acute bronchitis. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, eds. Feigin and Cherry's Textbook Of Pediatric Infectious Diseases. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 19.
Walsh EE. Acute bronchitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 65.
-
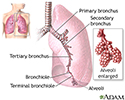
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Bronchitis - illustration
Bronchitis is the inflammation of the bronchi, the main air passages to the lungs. It often results from a respiratory infection caused by a virus or bacteria. Symptoms include coughing, shortness of breath, wheezing and fatigue.
Bronchitis
illustration
-
Causes of acute bronchitis - illustration
Bronchitis is an inflammation of the bronchial tubes, the part of the respiratory system that leads into the lungs. Acute bronchitis has a sudden onset and usually appears after a respiratory infection, such as a cold, and can be caused by either a virus or bacteria. The infection inflames the bronchial tubes, which causes symptoms such as fever, cough, sore throat, wheezing, and the production of thick yellow mucus. If acute bronchitis occurs because of a bacterial infection antibiotics are given for the treatment. Otherwise if the infection is viral medications can only be given to alleviate the symptoms. Although acute bronchitis is relatively common, some people are more prone to it than others.
Causes of acute bronchitis
illustration
-
Lung anatomy - illustration
When air is inhaled through the nose or mouth, it travels down the trachea to the bronchus, where it first enters the lung. From the bronchus, air goes through the bronchi, into the even smaller bronchioles and lastly into the alveoli.
Lung anatomy
illustration
-
Causes of chronic bronchitis - illustration
Chronic bronchitis is most frequently caused by long term irritation of the bronchial tubes. Bronchitis is considered chronic if symptoms continue for three months or longer. Bronchitis caused by allergies can also be classified as chronic bronchitis. Chronic bronchitis is caused most often by exposure to airborne pollutants such as cigarette smoke, excessive dust in the air, or chemicals. The bronchial lining becomes inflamed and the constant exposure to such pollutants begins to cause damage in the bronchioles (the smaller airways in the lungs). Symptoms of chronic bronchitis include shortness of breath or wheezing, chest pain, and chronic productive cough.
Causes of chronic bronchitis
illustration
-
COPD (chronic obstructive pulmonary disorder) - illustration
Chronic obstructive pulmonary disease (COPD) refers to chronic lung disorders that result in blocked air flow in the lungs. The two main COPD disorders are emphysema and chronic bronchitis, the most common causes of respiratory failure. Emphysema occurs when the walls between the lung's air sacs become weakened and collapse. Damage from COPD is usually permanent and irreversible.
COPD (chronic obstructive pulmonary disorder)
illustration
-
Pulse oximeter - illustration
A pulse oximeter is a small device that measures your blood oxygen level. It does this by using beams of light, without the need for a blood sample. When placed on your finger, the pulse oximeter analyzes the light that passes through your finger to determine the percentage of oxygen in your red blood cells. These devices can give an estimate of blood oxygen levels. Certain factors such as poor circulation, skin pigmentation, skin thickness or temperature, current tobacco use, and fingernail polish can all affect accuracy. For the best reading, make sure your finger is warm, relaxed, and held at a level below your heart. Remove any finger polish. Sit quietly during the reading. Your oxygen saturation level and heart rate will appear on a small screen on the top of the device. Pulse oximeters can be used monitor blood oxygen levels in case of illness such as COVID-19 or lung disease, such as asthma or COPD. Talk with your health care provider about how to use the pulse oximeter and what to do when levels drop too low.
Pulse oximeter
illustration
-
Lungs - illustration
The major features of the lungs include the bronchi, the bronchioles and the alveoli. The alveoli are the microscopic blood vessel-lined sacks in which oxygen and carbon dioxide gas are exchanged.
Lungs
illustration
-
Bronchitis - illustration
Bronchitis is the inflammation of the bronchi, the main air passages to the lungs. It often results from a respiratory infection caused by a virus or bacteria. Symptoms include coughing, shortness of breath, wheezing and fatigue.
Bronchitis
illustration
-
Causes of acute bronchitis - illustration
Bronchitis is an inflammation of the bronchial tubes, the part of the respiratory system that leads into the lungs. Acute bronchitis has a sudden onset and usually appears after a respiratory infection, such as a cold, and can be caused by either a virus or bacteria. The infection inflames the bronchial tubes, which causes symptoms such as fever, cough, sore throat, wheezing, and the production of thick yellow mucus. If acute bronchitis occurs because of a bacterial infection antibiotics are given for the treatment. Otherwise if the infection is viral medications can only be given to alleviate the symptoms. Although acute bronchitis is relatively common, some people are more prone to it than others.
Causes of acute bronchitis
illustration
-
Lung anatomy - illustration
When air is inhaled through the nose or mouth, it travels down the trachea to the bronchus, where it first enters the lung. From the bronchus, air goes through the bronchi, into the even smaller bronchioles and lastly into the alveoli.
Lung anatomy
illustration
-
Causes of chronic bronchitis - illustration
Chronic bronchitis is most frequently caused by long term irritation of the bronchial tubes. Bronchitis is considered chronic if symptoms continue for three months or longer. Bronchitis caused by allergies can also be classified as chronic bronchitis. Chronic bronchitis is caused most often by exposure to airborne pollutants such as cigarette smoke, excessive dust in the air, or chemicals. The bronchial lining becomes inflamed and the constant exposure to such pollutants begins to cause damage in the bronchioles (the smaller airways in the lungs). Symptoms of chronic bronchitis include shortness of breath or wheezing, chest pain, and chronic productive cough.
Causes of chronic bronchitis
illustration
-
COPD (chronic obstructive pulmonary disorder) - illustration
Chronic obstructive pulmonary disease (COPD) refers to chronic lung disorders that result in blocked air flow in the lungs. The two main COPD disorders are emphysema and chronic bronchitis, the most common causes of respiratory failure. Emphysema occurs when the walls between the lung's air sacs become weakened and collapse. Damage from COPD is usually permanent and irreversible.
COPD (chronic obstructive pulmonary disorder)
illustration
-
Pulse oximeter - illustration
A pulse oximeter is a small device that measures your blood oxygen level. It does this by using beams of light, without the need for a blood sample. When placed on your finger, the pulse oximeter analyzes the light that passes through your finger to determine the percentage of oxygen in your red blood cells. These devices can give an estimate of blood oxygen levels. Certain factors such as poor circulation, skin pigmentation, skin thickness or temperature, current tobacco use, and fingernail polish can all affect accuracy. For the best reading, make sure your finger is warm, relaxed, and held at a level below your heart. Remove any finger polish. Sit quietly during the reading. Your oxygen saturation level and heart rate will appear on a small screen on the top of the device. Pulse oximeters can be used monitor blood oxygen levels in case of illness such as COVID-19 or lung disease, such as asthma or COPD. Talk with your health care provider about how to use the pulse oximeter and what to do when levels drop too low.
Pulse oximeter
illustration
Review Date: 2/3/2024
Reviewed By: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.