Ectopic heartbeat
PVB (premature ventricular beat); Premature beats; PVC (premature ventricular complex/contraction); Extrasystole; Premature supraventricular contractions; PAC; Premature atrial contraction; Abnormal heartbeatEctopic heartbeats are changes in a heartbeat that is otherwise normal. These changes lead to extra or skipped heartbeats. There is often not a clear cause for these changes. They are common.
The two most common types of ectopic heartbeats are:
- Premature ventricular contractions (PVC)
- Premature atrial contractions (PAC)
Causes
Ectopic heartbeats are sometimes seen with:
- Changes in the blood, such as a low potassium level (hypokalemia)
Hypokalemia
Low blood potassium level is a condition in which the amount of potassium in the blood is lower than normal. The medical name of this condition is h...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Decrease in blood supply to the heart
-
When the heart is enlarged or structurally abnormal
When the heart is enlarged
Cardiomyopathy is disease in which the heart muscle becomes weakened, stretched, or has another structural problem. It often contributes to the hear...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Ectopic beats may be caused or made worse by smoking, alcohol use, caffeine, stimulant medicines, and some street drugs.
Alcohol use
Alcohol use involves drinking beer, wine, or hard liquor.
Caffeine
Caffeine is a substance that is found in certain plants. It can also be man-made and added to foods. It is a central nervous system stimulant and a...
Ectopic heartbeats are rare in children without heart disease that was present at birth (congenital). Most extra heartbeats in children are PACs. These are often benign.
In adults, ectopic heartbeats are common. They are most often due to PACs or PVCs. Your health care provider should look into the cause when they are frequent. Treatment is directed at symptoms and the underlying cause.
Symptoms
Symptoms include:
- Feeling your heartbeat (palpitations)
Palpitations
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Feeling like your heart stopped or skipped a beat
- Feeling of occasional, forceful beats
Note: There may be no symptoms.
Exams and Tests
A physical exam may show an occasional uneven pulse. If the ectopic heartbeats do not occur very often, your provider may not find them during a physical exam.
Physical exam
During a physical examination, a health care provider checks your body to determine if you do or do not have a physical problem. A physical examinati...

Blood pressure is most often normal.
An ECG will be done. Often, no further testing is needed when your ECG is normal and the symptoms are not severe or worrisome.
ECG
An electrocardiogram (ECG) is a test that records the electrical activity of the heart.

If your provider wants to know more about your heart rhythm, they may order:
- A monitor that you wear that records and stores your heart rhythm for 24 to 48 hours (Holter monitor)
Holter monitor
A Holter monitor is a machine that continuously records the heart's rhythms. The monitor is worn for 24 to 48 hours during normal activity.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - A recording device that you wear, and records your heart rhythm whenever you feel a skipped beat
An echocardiogram may be ordered if your provider suspects problems with the size or structure of your heart are the cause.
Echocardiogram
An echocardiogram is a test that uses sound waves to create pictures of the heart. The picture and information it produces is more detailed than a s...

Treatment
The following may help reduce ectopic heartbeats for some people:
- Limiting caffeine, alcohol, and tobacco
- Regular exercise for people who are inactive
For the most part, ectopic heartbeats do not need to be treated. The condition is only treated if your symptoms are severe or if the extra beats occur very often.
The cause of the heartbeats, if it can be found, may also need to be treated.
Outlook (Prognosis)
In some cases, ectopic heartbeats may mean you are at greater risk for serious abnormal heart rhythms, such as ventricular tachycardia.
Ventricular tachycardia
Ventricular tachycardia (VT) is a rapid heartbeat that starts in the lower chambers of the heart (ventricles).

When to Contact a Medical Professional
Contact your provider if:
- You keep feeling the sensation of your heart pounding or racing (palpitations).
Palpitations
Palpitations are feelings or sensations that your heart is pounding or racing. They can be felt in your chest, throat, or neck. You may:Have an unpl...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You have palpitations with chest pain or other symptoms.
Chest pain
Chest pain is discomfort or pain that you feel anywhere along the front of your body between your neck and upper abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You have this condition and your symptoms get worse or do not improve with treatment.
References
Fang JC, O'Gara PT. History and physical examination: an evidence-based approach. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 13.
Olgin JE. Approach to the patient with suspected arrhythmias. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 49.
-
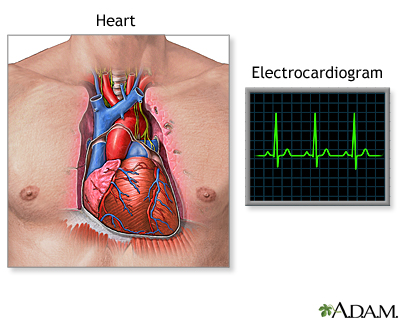
Heart - section through the middle - illustration
The interior of the heart is composed of valves, chambers, and associated vessels.
Heart - section through the middle
illustration
-
Heart - front view - illustration
The external structures of the heart include the ventricles, atria, arteries and veins. Arteries carry blood away from the heart while veins carry blood into the heart. The vessels colored blue indicate the transport of blood with relatively low content of oxygen and high content of carbon dioxide. The vessels colored red indicate the transport of blood with relatively high content of oxygen and low content of carbon dioxide.
Heart - front view
illustration
-
Electrocardiogram (ECG) - illustration
An electrocardiogram is a test that measures the electrical activity of the heart. This includes the rate and regularity of beats as well as the size and position of the chambers, any damage to the heart, and effects of drugs or devices to regulate the heart.
Electrocardiogram (ECG)
illustration
-
Heart - section through the middle - illustration
The interior of the heart is composed of valves, chambers, and associated vessels.
Heart - section through the middle
illustration
-
Heart - front view - illustration
The external structures of the heart include the ventricles, atria, arteries and veins. Arteries carry blood away from the heart while veins carry blood into the heart. The vessels colored blue indicate the transport of blood with relatively low content of oxygen and high content of carbon dioxide. The vessels colored red indicate the transport of blood with relatively high content of oxygen and low content of carbon dioxide.
Heart - front view
illustration
-
Electrocardiogram (ECG) - illustration
An electrocardiogram is a test that measures the electrical activity of the heart. This includes the rate and regularity of beats as well as the size and position of the chambers, any damage to the heart, and effects of drugs or devices to regulate the heart.
Electrocardiogram (ECG)
illustration
Review Date: 5/8/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.