Hepatitis
Hepatitis is swelling and inflammation of the liver.
Causes
Hepatitis can be caused by:
-
Immune cells in the body attacking the liver (autoimmune hepatitis)
Immune cells in the body attacking the ...
Autoimmune hepatitis causes inflammation of the liver. It occurs when immune cells mistake the liver's normal cells for harmful invaders and attack ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Infections from viruses (such as hepatitis A, hepatitis B, or hepatitis C), bacteria, or parasites
- Liver damage from alcohol or poison
- Medicines, such as an overdose of acetaminophen
- Fatty liver
Liver disease can also be caused by inherited disorders such as cystic fibrosis or hemochromatosis, a condition that involves having too much iron in your body.
Other causes include Wilson disease, a disorder in which the body retains too much copper and ingestion of toxic mushrooms.
Symptoms
Hepatitis may start and get better quickly. It may also become a long-term condition. In some cases, hepatitis may lead to liver damage, liver failure, cirrhosis, liver cancer, or even death.
There are several factors that can affect how severe the condition is. These may include the cause of the liver damage and any illnesses you have. Hepatitis A, for example, is most often short-term and does not lead to chronic liver problems.
The symptoms of hepatitis include:
- Pain or bloating in the belly area
- Dark urine and pale or clay-colored stools
- Fatigue
- Low grade fever
- Itching
- Jaundice (yellowing of the skin or eyes)
- Loss of appetite
- Nausea and vomiting
- Weight loss
You may not have symptoms when first infected with hepatitis B or C. You can still develop liver failure later. If you have any risk factors for either type of hepatitis, ask your health care provider whether you should be tested for them.
Exams and Tests
You will have a physical exam to look for:
- Enlarged and tender liver
- Fluid in the abdomen (ascites)
- Yellowing of the skin
You may have lab tests to diagnose and monitor your condition, including:
- Ultrasound, MRI, or other imaging of the abdomen
- Autoimmune and other blood markers
- Blood tests to diagnose Hepatitis A, B, or C or other viruses that cause hepatitis
- Liver function tests and liver enzymes
- Liver biopsy to check for liver damage (may be needed in some cases)
- Paracentesis (if fluid is in your abdomen)
Treatment
Your provider will talk to you about treatment options. Treatments will vary, depending on the cause of your liver disease. You may need to eat a high-calorie diet if you are losing weight.
Support Groups
More information and support for people with hepatitis and their families can be found by joining a support group. Ask your provider about liver disease resources and support groups in your area.
Outlook (Prognosis)
The outlook for hepatitis will depend on what is causing the liver damage and how severely the hepatitis has affected your liver.
Possible Complications
Complications may include:
- Permanent liver damage, called cirrhosis
- Liver failure
- Liver cancer
When to Contact a Medical Professional
Seek care immediately if you:
- Have symptoms from too much acetaminophen or other medicines. You may need to have your stomach pumped
- Vomit blood
- Have bloody or tarry stools
- Are confused or delirious
Contact your provider if:
- You have any symptoms of hepatitis or believe that you have been exposed to hepatitis A, B, or C.
- You cannot keep food down due to excessive vomiting. You may need to receive nutrition through a vein (intravenously).
- You feel sick and have traveled to Asia, Africa, South America, or Central America.
Prevention
Talk to your provider about having a vaccine to prevent hepatitis A and hepatitis B.
Avoid alcohol. Treat any underlying conditions that can lead to liver disease, including overweight/obesity, diabetes, high blood pressure, and other metabolic disorders.
Steps for preventing the spread of hepatitis B and C from one person to another include:
- Avoid sharing personal items, such as razors or toothbrushes.
- DO NOT share drug needles or other drug equipment (such as straws for snorting drugs).
- Clean blood spills with a mixture of 1 part household bleach to 9 parts water.
- DO NOT get tattoos or body piercings with instruments that have not been cleaned properly.
- Use safer sexual practices.
To reduce your risk for spreading or catching hepatitis A:
- Always wash your hands well after using the restroom, and when you come in contact with an infected person's blood, stools, or other bodily fluid.
- Avoid unclean food and water.
References
Centers for Disease Control and Prevention website. Viral hepatitis surveillance and case management. www.cdc.gov/hepatitis/php/surveillance-guidance/. Updated February 29, 2024. Accessed October 29, 2025.
Czaja AJ. Autoimmune hepatitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 90.
Pawlotsky J-M. Chronic viral and autoimmune hepatitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 135.
Takyar V, Ghany MG. Hepatitis A, B, D, and E. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:237-244.
Young J-A H, Ustun C. Infections in recipients of hematopoietic stem cell transplants. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 307.
-
Hepatitis B virus - illustration
Hepatitis B is also known as serum hepatitis and is spread through blood and sexual contact. It is seen with increased frequency among intravenous drug users who share needles and among the homosexual population. This photograph is an electronmicroscopic image of hepatitis B virus particles. (Image courtesy of the Centers for Disease Control and Prevention.)
Hepatitis B virus
illustration
-
Hepatitis C - illustration
Hepatitis C is a virus-caused liver inflammation which may cause jaundice, fever and cirrhosis. Persons who are most at risk for contracting and spreading hepatitis C are those who share needles for injecting drugs and health care workers or emergency workers who may be exposed to contaminated blood.
Hepatitis C
illustration
-
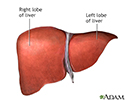
Liver anatomy - illustration
The liver serves a wide variety of body functions, including detoxifying blood and producing bile that aids in digestion.
Liver anatomy
illustration
-
Cirrhosis of the liver - illustration
A chronic liver disease which causes damage to liver tissue, scarring of the liver (fibrosis; nodular regeneration), progressive decrease in liver function, excessive fluid in the abdomen (ascites), bleeding disorders (coagulopathy), increased pressure in the blood vessels (portal hypertension), and brain function disorders (hepatic encephalopathy). Excessive alcohol use is the leading cause of cirrhosis.
Cirrhosis of the liver
illustration
-
Hepatitis B virus - illustration
Hepatitis B is also known as serum hepatitis and is spread through blood and sexual contact. It is seen with increased frequency among intravenous drug users who share needles and among the homosexual population. This photograph is an electronmicroscopic image of hepatitis B virus particles. (Image courtesy of the Centers for Disease Control and Prevention.)
Hepatitis B virus
illustration
-
Hepatitis C - illustration
Hepatitis C is a virus-caused liver inflammation which may cause jaundice, fever and cirrhosis. Persons who are most at risk for contracting and spreading hepatitis C are those who share needles for injecting drugs and health care workers or emergency workers who may be exposed to contaminated blood.
Hepatitis C
illustration
-
Liver anatomy - illustration
The liver serves a wide variety of body functions, including detoxifying blood and producing bile that aids in digestion.
Liver anatomy
illustration
-
Cirrhosis of the liver - illustration
A chronic liver disease which causes damage to liver tissue, scarring of the liver (fibrosis; nodular regeneration), progressive decrease in liver function, excessive fluid in the abdomen (ascites), bleeding disorders (coagulopathy), increased pressure in the blood vessels (portal hypertension), and brain function disorders (hepatic encephalopathy). Excessive alcohol use is the leading cause of cirrhosis.
Cirrhosis of the liver
illustration
Review Date: 3/31/2024
Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.