Anorchia
Vanishing testes - anorchia; Empty scrotum - anorchia; Scrotum - empty (anorchia)Anorchia is the absence of both testes at birth.
Testes
The testes are 2 egg-shaped male reproductive organs located in the scrotum. They produce sperm and the male hormone, testosterone.

Causes
An embryo develops early sex organs in the first several weeks of pregnancy. In some cases, early testes do not develop in males before 8 weeks into the pregnancy. These babies will be born with female sex organs.
In some cases, the testes disappear between 8 and 10 weeks. These babies will be born with ambiguous genitalia. This means the child will have parts of both male and female sex organs.
Ambiguous genitalia
Ambiguous genitalia is a rare condition where a child is born with outer genitals that do not clearly look either male or female. They may have feat...

In some cases, the testes may disappear between 12 and 14 weeks. These babies will have a normal penis and scrotum. However, they will not have any testes. This is known as congenital anorchia. It is also called the "vanishing testes syndrome."
The cause is unknown. Genetic factors may be involved in some cases.
This condition should not be confused with bilateral undescended testes, in which the testes are located in the abdomen or groin rather than the scrotum.
Bilateral undescended testes
Undescended testicle occurs when one or both testicles fail to move into the scrotum before birth.

Symptoms
Symptoms may include:
- Normal outside genitals before puberty
- Failure to start puberty at the correct time
Puberty
Puberty is when your body changes, when you develop from being a boy to a man. Learn what changes to expect so that you feel more prepared....
Read Article Now Book Mark Article
Exams and Tests
Signs include:
- Empty scrotum
- Lack of male sex characteristics (penis and pubic hair growth, deepening of the voice, and increase in muscle mass)
Tests include:
- Anti-Müllerian hormone levels
-
Bone density
Bone density
A bone mineral density (BMD) test measures how much calcium and other types of minerals are in an area of your bone. This test helps your health care...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Follicle stimulating hormone (FSH) and luteinizing hormone (LH) levels
Follicle stimulating hormone
The follicle stimulating hormone (FSH) blood test measures the level of FSH in blood. FSH is a hormone released by the pituitary gland, located on t...
Read Article Now Book Mark ArticleLuteinizing hormone
The luteinizing hormone (LH) blood test measures the amount of LH in blood. LH is a hormone released by the pituitary gland, located on the undersid...
Read Article Now Book Mark Article - Surgery to look for male reproductive tissue
-
Testosterone levels (low)
Testosterone levels
A testosterone test measures the amount of the male hormone, testosterone, in the blood. Both men and women produce this hormone. The test described...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Ultrasound or magnetic resonance imaging (MRI) to look for testes in the abdomen
Ultrasound
Ultrasound uses high-frequency sound waves to make images of organs and structures inside the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleMagnetic resonance imaging
A magnetic resonance imaging (MRI) scan is an imaging test that uses powerful magnets and radio waves to create pictures of the body. It does not us...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - XY karyotype
Treatment
Treatment includes:
- Artificial (prosthetic) testicle implants
- Male hormones (androgens)
- Psychological support
Outlook (Prognosis)
The outlook is good with treatment.
Possible Complications
Complications include:
- Face, neck, or back abnormalities in some cases
- Infertility
- Psychological issues
When to Contact a Medical Professional
Contact your health care provider if a male child:
- Appears to have extremely small or absent testicles
- Does not seem to be starting puberty during his early teens
References
Ali O, Donohoue PA. Hypofunction of the testes. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 623.
Chan Y-M, Hannema SE. Differences of sex development. In: Melmed S, Auchus RJ, Goldfine AB, Rosen CJ, Kopp PA, eds. Williams Textbook of Endocrinology. 15th ed. Philadelphia, PA: Elsevier; 2025:chap 21.
Yu RN, Diamond DA. Disorders of sexual development: etiology, evaluation, and medical management. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 48.
-
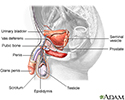
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
-
Male reproductive anatomy - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive anatomy
illustration
-
Male reproductive system - illustration
The male reproductive structures include the penis, the scrotum, the testicles (testes), the epididymis, the seminal vesicles, and the prostate.
Male reproductive system
illustration
Review Date: 9/2/2024
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/05/2025.