Arthritis
Joint inflammation; Joint degenerationArthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis.
Causes
Arthritis involves the breakdown of structures of the joint, particularly cartilage. Normal cartilage protects a joint and allows it to move smoothly. Cartilage also absorbs shock when pressure is placed on the joint, such as when you walk. Without the normal amount of cartilage, the bones under the cartilage become damaged and rub together. This causes swelling (inflammation), and stiffness.
Other joint structures affected by arthritis include:
- The synovium
- The bone next to the joint
- Ligaments and tendons
- Sacs that may be fluid-filled next to bone, ligaments and tendons (bursae)
Joint inflammation and damage may result from:
- An autoimmune disease (the body's immune system mistakenly attacks healthy tissue)
- Broken bone
- General "wear and tear" on joints
- Infection, most often by bacteria or viruses
- Crystals such as uric acid or calcium pyrophosphate dihydrate
In most cases, the joint inflammation goes away after the cause goes away or is treated. Sometimes, it does not. When this happens, you have long-term (chronic) arthritis.
Arthritis may occur in people of any age and sex. Osteoarthritis, which is due to non-inflammatory processes and increases with age, is the most common type.
Osteoarthritis
Osteoarthritis (OA) is the most common joint disorder. It is due to aging and wear and tear on a joint.

Other, more common types of inflammatory arthritis include:
-
Ankylosing spondylitis
Ankylosing spondylitis
Ankylosing spondylitis (AS) is a chronic form of arthritis. It mostly affects the bones and joints at the base of the spine where it connects with t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Crystal arthritis, gout, calcium pyrophosphate deposition disease
-
Juvenile rheumatoid arthritis (in children)
Juvenile rheumatoid arthritis
Juvenile idiopathic arthritis (JIA) is a term used to describe a group of disorders in children that includes arthritis. They are long-term (chronic...
Read Article Now Book Mark Article - Bacterial infections
-
Psoriatic arthritis
Psoriatic arthritis
Psoriatic arthritis is a joint problem (arthritis) that often occurs with a skin condition called psoriasis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Reactive arthritis
Reactive arthritis
Reactive arthritis is a type of arthritis that follows an infection. It may also cause inflammation of the eyes, skin and urinary and genital system...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Rheumatoid arthritis (in adults)
Rheumatoid arthritis
Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also aff...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Scleroderma
Scleroderma
Scleroderma is a disease that involves the buildup of fibrous tissue in the skin and elsewhere in the body. It also damages the cells that line the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Systemic lupus erythematosus (SLE)
Systemic lupus erythematosus
Systemic lupus erythematosus (SLE) is an autoimmune disease. In this disease, the immune system of the body mistakenly attacks healthy tissue. It c...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Symptoms
Arthritis causes joint pain, swelling, stiffness, and limited movement. Symptoms can include:
- Joint pain
-
Joint swelling
Joint swelling
Joint swelling is the buildup of fluid in the soft tissue surrounding the joint or the joint itself.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Joint deformity
- Reduced ability to move the joint
- Redness and warmth of the skin around a joint
- Joint stiffness, especially in the morning
Exams and Tests
The health care provider will perform a physical exam and ask about your medical history.
The physical exam may show:
- Fluid in or around a joint
- Warm, red, tender joints
- Difficulty moving a joint (called "limited range of motion")
Some types of arthritis may cause joint deformity. This may be a sign of severe, untreated rheumatoid arthritis or of osteoarthritis.
Blood tests and joint x-rays are often done to check for infection and other causes of arthritis.
Joint x-rays
This test is an x-ray of a knee, shoulder, hip, wrist, ankle, or other joint.

The provider may also remove a sample of joint fluid with a needle and send it to a lab to be checked for inflammation crystals or infection.
Treatment
The underlying cause often cannot be cured. The goal of treatment is to:
- Reduce pain and inflammation
- Improve function
- Prevent further joint damage
LIFESTYLE CHANGES
Lifestyle changes are the preferred treatment for osteoarthritis and other types of joint swelling. Exercise can help relieve stiffness, reduce pain and fatigue, and improve muscle and bone strength. Your health care team can help you design an exercise program that is best for you.
Exercise program
When you have arthritis, being active is good for your overall health and sense of well-being. Exercise keeps the muscles around your joints strong a...

Exercise programs may include:
- Low-impact aerobic activity (also called endurance exercise) such as walking
- Range of motion exercises for flexibility
- Strength training for muscle tone
Your provider may suggest physical therapy. This might include:
- Heat or ice.
- Splints or orthotics to support joints and help improve their position. This is often needed for rheumatoid arthritis.
- Water therapy.
- Massage.
Other things you can do include:
- Get plenty of sleep. Sleeping 8 to 10 hours a night and taking naps during the day can help you recover from a flare-up more quickly, and may even help prevent flare-ups.
- Avoid staying in one position for too long.
- Avoid positions or movements that place extra stress on your sore joints.
-
Change your home to make activities easier. For example, install grab bars in the shower, the tub, and near the toilet.
Change your home
As the pain from arthritis becomes worse, keeping up with everyday activities may become more difficult. Making changes around your home will take so...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Try stress-reducing activities, such as meditation, yoga, or tai chi.
- Eat a healthy diet with plenty of fruits and vegetables, which contain important vitamins and minerals.
- Eat foods rich in omega-3 fatty acids, such as cold-water fish (salmon, mackerel, and herring), flaxseed, rapeseed (canola) oil, soybeans, soybean oil, pumpkin seeds, and walnuts.
- Avoid smoking and excessive alcohol consumption.
- Apply capsaicin cream over your painful joints. You may feel improvement after applying the cream for 3 to 7 days.
- Lose weight, if you are overweight. Weight loss can greatly improve joint pain in the legs and feet.
- Use a cane to reduce pain from hip, knee, ankle, or foot arthritis.
MEDICINES
Medicines may be prescribed along with lifestyle changes. All medicines have some risks. You should be closely followed by a provider when taking arthritis medicines, even ones you buy over-the-counter.
Arthritis medicines
The pain, swelling, and stiffness of arthritis can limit your movement. Medicines can help manage your symptoms so that you can continue to lead an ...

Over-the-counter medicines:
- Acetaminophen (Tylenol) is often the first medicine tried to reduce pain. Take up to 3,000 mg a day (2 extra-strength Tylenol every 8 hours). To prevent damage to your liver, do not take more than the recommended dose. Since multiple medicines are available without a prescription that also contain acetaminophen, you will need to include them in the 3,000 mg per day maximum. Also, avoid alcohol when taking acetaminophen.
- Aspirin, ibuprofen, or naproxen are nonsteroidal anti-inflammatory drugs (NSAIDs) that can relieve arthritis pain. However, they can carry risks when used for a long time. Possible side effects include heart attack, stroke, stomach ulcers, bleeding from the digestive tract, and kidney damage.
Depending on the type of arthritis, a number of other medicines may be prescribed:
- Corticosteroids ("steroids") help reduce inflammation. They may be injected into painful joints or given by mouth.
- Disease-modifying anti-rheumatic drugs (DMARDs) are used to treat autoimmune arthritis and SLE
- Biologics and kinase inhibitors are used for the treatment of autoimmune arthritis. They may be given by injection or by mouth.
- For gout, certain medicines to lower uric acid levels may be used.
It is very important to take your medicines as directed by your provider. If you are having problems doing so (for example, because of side effects), you should talk to your provider. Also make sure your provider knows about all the medicines you are taking, including vitamins and supplements bought without a prescription.
SURGERY AND OTHER TREATMENTS
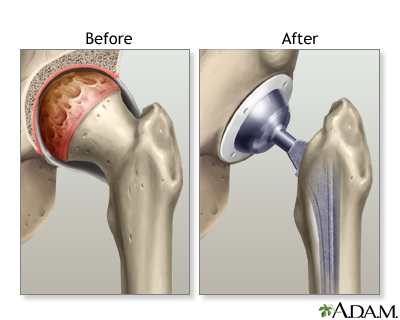
In some cases, surgery may be done if other treatments have not worked and severe damage to a joint occurs.
This may include:
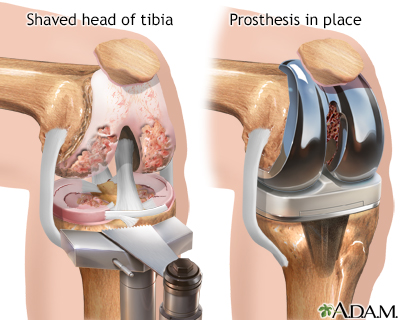
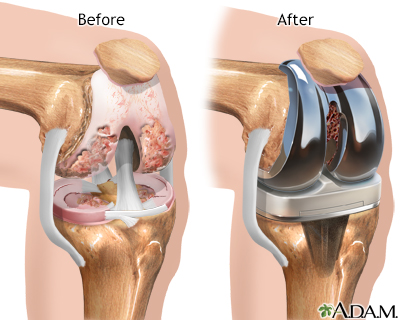
- Joint replacement, such as a total knee joint replacement
Total knee joint replacement
Knee joint replacement is a surgery to replace a knee joint with a man-made artificial joint. The artificial joint is called a prosthesis.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Outlook (Prognosis)
A few arthritis-related disorders can be completely cured with proper treatment. Yet, many of these disorders become long-term (chronic) health problems but can often be well-controlled. Aggressive forms of some arthritic conditions may have significant effects on mobility and may lead to involvement of other body organs or systems.
Possible Complications
Complications of arthritis include:
- Long-term (chronic) pain
- Disability
- Difficulty performing daily activities
When to Contact a Medical Professional
Contact your provider if:
- Your joint pain persists beyond 3 days.
- You have severe unexplained joint pain.
- The affected joint is significantly swollen.
- You have a hard time moving the joint.
- Your skin around the joint is red or hot to the touch.
- You have a fever or have lost weight unintentionally.
Prevention
Early diagnosis and treatment can help prevent joint damage. If you have a family history of arthritis, tell your provider, even if you do not have joint pain.
Avoiding excessive, repeated motions may help protect you against osteoarthritis.
References
Bykerk VP, Crow MK. Approach to the patient with rheumatic disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 236.
Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2021;73(7):1108-1123. PMID: 34101376 pubmed.ncbi.nlm.nih.gov/34101376/.
Hunter DJ. Osteoarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 241.
Inman RD, Rahman P. Spondyloarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 244.
McInnes IB. Rheumatoid arthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 243.
-
Arthritis
Animation
-
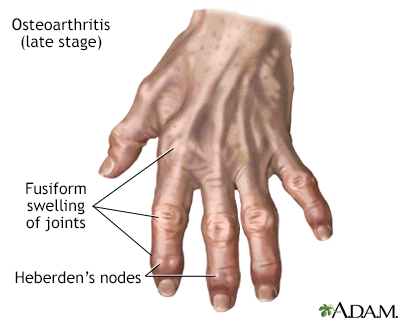
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
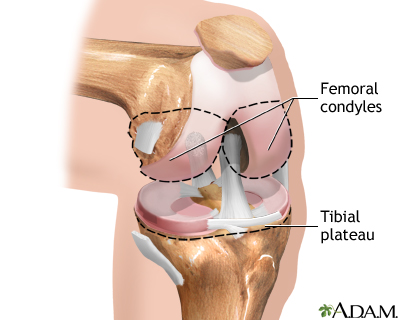
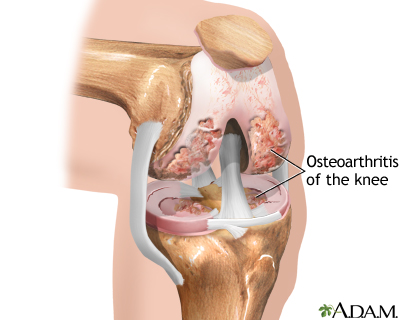
Osteoarthritis - illustration
Osteoarthritis is associated with the aging process and can affect any joint. The cartilage of the affected joint is gradually worn down, eventually causing bone to rub against bone. Bony spurs develop on the unprotected bones causing pain and inflammation.
Osteoarthritis
illustration
-
Rheumatoid arthritis - illustration
Rheumatoid arthritis is an autoimmune disease in which the body's immune system attacks itself. The pattern of joints affected is usually symmetrical, involves the hands and other joints and is worse in the morning. Rheumatoid arthritis is also a systemic disease, involving other body organs, whereas osteoarthritis is limited to the joints. Over time, both forms of arthritis can be crippling.
Rheumatoid arthritis
illustration
-
Rheumatoid arthritis - illustration
The affect of rheumatoid arthritis can progress to the degree that it is crippling. Deformities distinctive to late-stage rheumatoid arthritis such as ulnar deviation of the bones of the hands, or swan-neck deviation of the fingers occur because muscles and tendons on one side of the joint may overpower those on the other side, pulling the bones out of alignment.
Rheumatoid arthritis
illustration
-
Osteoarthritis vs. rheumatoid arthritis - illustration
Osteoarthritis is a deterioration of cartilage and overgrowth of bone often due to wear and tear. Rheumatoid arthritis is the inflammation of a joint's connective tissues, such as the synovial membranes, which leads to the destruction of the articular cartilage.
Osteoarthritis vs. rheumatoid arthritis
illustration
-
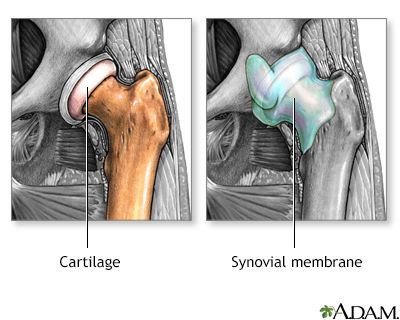
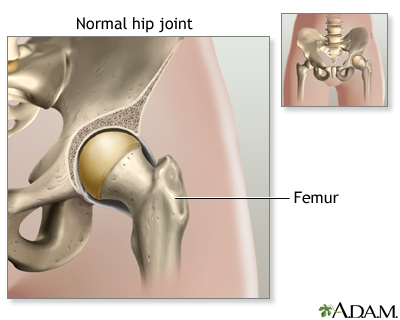
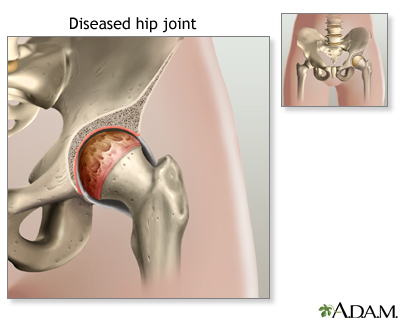
Arthritis in hip - illustration
Cartilage normally protects the joint, allowing for smooth movement. Cartilage also absorbs shock when pressure is placed on the joint, like when walking. Arthritis involves the breakdown of cartilage. Without the usual amount of cartilage, the bones of the joint rub together, causing pain, swelling and stiffness.
Arthritis in hip
illustration
-
Rheumatoid arthritis - illustration
Rheumatoid arthritis is another form of arthritis. The body's own immune system attacks a joint's synovial membrane, which secretes fluid and lines the joint. The synovium becomes inflamed, produces excess fluid, and the cartilage becomes rough and pitted.
Rheumatoid arthritis
illustration
-
Knee joint replacement - Series
Presentation
-
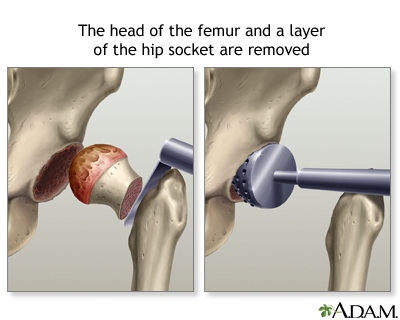
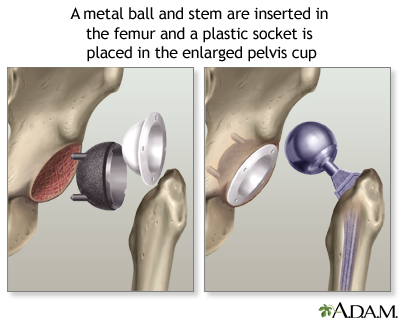
Hip joint replacement - Series
Presentation
-
Osteoarthritis - illustration
Osteoarthritis is a chronic disease of the joint cartilage and bone, often thought to result from wear and tear on a joint, although there are other causes such as congenital defects, trauma and metabolic disorders. Joints appear larger, are stiff and painful and usually feel worse the more they are used throughout the day.
Osteoarthritis
illustration
-
Osteoarthritis - illustration
Osteoarthritis is associated with the aging process and can affect any joint. The cartilage of the affected joint is gradually worn down, eventually causing bone to rub against bone. Bony spurs develop on the unprotected bones causing pain and inflammation.
Osteoarthritis
illustration
-
Rheumatoid arthritis - illustration
Rheumatoid arthritis is an autoimmune disease in which the body's immune system attacks itself. The pattern of joints affected is usually symmetrical, involves the hands and other joints and is worse in the morning. Rheumatoid arthritis is also a systemic disease, involving other body organs, whereas osteoarthritis is limited to the joints. Over time, both forms of arthritis can be crippling.
Rheumatoid arthritis
illustration
-
Rheumatoid arthritis - illustration
The affect of rheumatoid arthritis can progress to the degree that it is crippling. Deformities distinctive to late-stage rheumatoid arthritis such as ulnar deviation of the bones of the hands, or swan-neck deviation of the fingers occur because muscles and tendons on one side of the joint may overpower those on the other side, pulling the bones out of alignment.
Rheumatoid arthritis
illustration
-
Osteoarthritis vs. rheumatoid arthritis - illustration
Osteoarthritis is a deterioration of cartilage and overgrowth of bone often due to wear and tear. Rheumatoid arthritis is the inflammation of a joint's connective tissues, such as the synovial membranes, which leads to the destruction of the articular cartilage.
Osteoarthritis vs. rheumatoid arthritis
illustration
-
Arthritis in hip - illustration
Cartilage normally protects the joint, allowing for smooth movement. Cartilage also absorbs shock when pressure is placed on the joint, like when walking. Arthritis involves the breakdown of cartilage. Without the usual amount of cartilage, the bones of the joint rub together, causing pain, swelling and stiffness.
Arthritis in hip
illustration
-
Rheumatoid arthritis - illustration
Rheumatoid arthritis is another form of arthritis. The body's own immune system attacks a joint's synovial membrane, which secretes fluid and lines the joint. The synovium becomes inflamed, produces excess fluid, and the cartilage becomes rough and pitted.
Rheumatoid arthritis
illustration
-
Knee joint replacement - Series
Presentation
-
Hip joint replacement - Series
Presentation
Review Date: 12/31/2023
Reviewed By: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.