Rabies
Hydrophobia; Animal bite - rabies; Dog bite - rabies; Bat bite - rabies; Raccoon bites - rabiesRabies is a deadly viral infection that is mainly spread by infected animals.
Causes
This infection is caused by the rabies virus. Rabies is spread by infected saliva that enters the body through a bite or broken skin. The virus travels from the wound to the brain, where it causes swelling or inflammation. This inflammation leads to symptoms of the disease. Most rabies deaths occur in children.
In the past, human rabies cases in the United States usually resulted from a dog bite. Recently, more cases of human rabies have been linked to bats and raccoons. Dog bites are a common cause of rabies in developing countries, especially Asia and Africa. There have been no reports of rabies caused by dog bites in the United States for a number of years due to widespread animal vaccination.
Other wild animals that can spread the rabies virus include:
- Foxes
- Skunks
Bats can spread rabies through minor or unrecognized bites or scratches. Bites can be so small you may not realize you have been bitten. If you find a bat in your home, you should contact your health care provider or health department, even if you don't feel or see a bite. They can advise you about whether you need treatment.
In rare cases, rabies has been transmitted without an actual bite. This type of infection is believed to be caused by infected saliva or other infectious material that may come in contact with an existing scratch or wound, usually in bat caves.
Symptoms
The time between infection and when you get sick ranges from 10 days to 7 years. This time period is called the incubation period. The average incubation period is 3 to 12 weeks.
Fear of water (hydrophobia) is the most common symptom. Other symptoms may include:
- Drooling
-
Headache
Headache
A headache is pain or discomfort in the head, scalp, or neck. Serious causes of headaches are rare. Most people with headaches can feel much better...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Seizures
Seizures
A seizure is the physical changes in behavior that occurs during an episode of specific types of abnormal electrical activity in the brain. The term ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bite site is very sensitive
- Mood changes
- Nausea and vomiting
- Loss of feeling in an area of the body
- Loss of muscle function
-
Fever (102°F or 38.8°C, or lower)
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Muscle spasms
Muscle spasms
Muscle cramps are when a muscle gets tight (contracts) without you trying to tighten it, and it does not relax. Cramps may involve all or part of on...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Numbness and tingling
Numbness and tingling
Numbness and tingling are abnormal sensations that can occur anywhere in your body, but they are often felt in your fingers, hands, feet, arms, or le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pain at the site of the bite
-
Restlessness
Restlessness
Agitation is an unpleasant state of extreme arousal. An agitated person may feel stirred up, excited, tense, confused, or irritable.
Read Article Now Book Mark Article - Swallowing difficulty (drinking causes spasms of the voice box)
-
Hallucinations
Hallucinations
Hallucinations involve sensing things such as visions, sounds, or smells that seem real but are not. These things are created by the mind.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
If an animal bites you, try to gather as much information about the animal as possible. Call your local animal control authorities to safely capture the animal. If rabies is suspected, the animal will be watched for signs of rabies.
A special test called immunofluorescence is used to look at the brain tissue after an animal is dead. This test can reveal whether the animal had rabies.
Your provider will examine you and look at the bite. The wound will be cleaned and treated.
The same test used on animals can be done to check for rabies in humans. The test uses a piece of skin from the neck. Your provider may also look for the rabies virus in your saliva or spinal fluid, although these tests are not as sensitive and may need to be repeated.
A spinal tap may be done to look for signs of the infection in your spinal fluid. Other tests done may include:
Spinal tap
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...

-
MRI of brain
MRI of brain
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
CT of the head
CT of the head
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
The aim of treatment is to relieve the symptoms of the bite wound and assess risk of rabies infection. Clean the wound well with soap and water and seek professional medical help. You will need your provider to clean the wound and remove any foreign objects. Most of the time, stitches should not be used for animal bite wounds.
If there is any risk of rabies, you will be given a series of a preventive vaccine. The vaccine is generally given in 4 doses over 14 days. Antibiotics have no effect on the rabies virus.
Vaccine
Vaccines are used to boost your immune system, reduce the risk of infection, and lessen the severity of infections, including those that cause seriou...

Most people also receive a treatment called human rabies immunoglobulin (HRIG). This treatment is given the day the bite occurred.
Contact your provider right away after an animal bite or after being exposed to animals such as bats, foxes, and skunks. They may carry rabies.
- Contact your provider even when no bite took place.
- Immunization and treatment for possible rabies are recommended for at least up to 14 days after exposure or a bite.
There is no known curative treatment for people with symptoms of a rabies infection. It is nearly always a fatal illness, but there have been a few reports of people surviving with experimental treatments.
Outlook (Prognosis)
It is possible to prevent rabies if you get the vaccine soon after the bite. To date, no one in the United States has developed rabies when they were given the vaccine promptly and appropriately.
Once the symptoms appear, the person rarely survives the disease, even with treatment. Death from respiratory failure usually occurs within 7 days after symptoms start.
Respiratory
The words "respiratory" and "respiration" refer to the lungs and breathing.

Possible Complications
Rabies is a life-threatening infection. Left untreated, rabies usually leads to coma and death.
In rare cases, some people may have an allergic reaction to the rabies vaccine.
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if an animal bites you.
Prevention
To help prevent rabies:
- Avoid contact with animals you don't know.
- Get vaccinated if you work in a high-risk occupation or travel to countries with a high rate of rabies.
- Make sure your pets receive the proper immunizations. Ask your veterinarian.
- Make sure that your pet does not come in contact with any wild animals.
- Follow quarantine regulations on importing dogs and other mammals in disease-free countries.
References
Centers for Disease Control and Prevention website. Rabies. About rabies. www.cdc.gov/rabies/about/index.html. Updated June 21, 2024. Accessed September 10, 2024.
Seethala R, Takhar SS, Bullard-Berent J, Banks LL. Viruses. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 119.
Williams B, Rupprecht CE, Bleck TP. Rabies (rhabdoviruses). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 163.
-
Rabies - illustration
Rabies is an acute viral infection is transmitted to humans by a bite or by the exposure of broken skin to an infected animal's saliva. Immunization given early (preferably within 24 hours but certainly within 72 hours) can usually prevent the disease.
Rabies
illustration
-
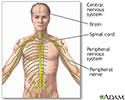
Central nervous system and peripheral nervous system - illustration
The central nervous system is made up of the brain and the spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
-
Rabies - illustration
The central nervous system is made up of the brain and spinal cord. The brain functions to receive nerve impulses from the spinal cord and cranial nerves. The spinal cord contains the nerves that carry messages between the brain and the body. The rabies virus spreads through the nerves, first causing flu-like symptoms such as fever and malaise. As the disease advances to the brain, it causes anxiety, confusion, brain dysfunction, progressing to hallucinations, delirium, and insomnia. If left untreated, rabies is nearly always fatal.
Rabies
illustration
-
Rabies - illustration
Rabies is an acute viral infection is transmitted to humans by a bite or by the exposure of broken skin to an infected animal's saliva. Immunization given early (preferably within 24 hours but certainly within 72 hours) can usually prevent the disease.
Rabies
illustration
-
Central nervous system and peripheral nervous system - illustration
The central nervous system is made up of the brain and the spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
-
Rabies - illustration
The central nervous system is made up of the brain and spinal cord. The brain functions to receive nerve impulses from the spinal cord and cranial nerves. The spinal cord contains the nerves that carry messages between the brain and the body. The rabies virus spreads through the nerves, first causing flu-like symptoms such as fever and malaise. As the disease advances to the brain, it causes anxiety, confusion, brain dysfunction, progressing to hallucinations, delirium, and insomnia. If left untreated, rabies is nearly always fatal.
Rabies
illustration
Review Date: 8/29/2024
Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.