Anti-reflux surgery
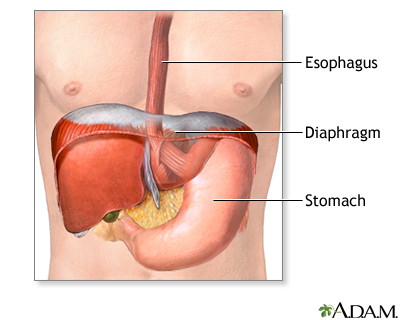
Fundoplication; Nissen fundoplication; Belsey (Mark IV) fundoplication; Toupet fundoplication; Thal fundoplication; Hiatal hernia repair; Endoluminal fundoplication; Gastroesophageal reflux - surgery; GERD - surgery; Reflux - surgery; Hiatal hernia - surgeryAnti-reflux surgery is a treatment for acid reflux, also known as GERD (gastroesophageal reflux disease). GERD is a condition in which food or stomach acid comes back up from your stomach into the esophagus. The esophagus is the tube from your mouth to the stomach.
GERD
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backward from the stomach into the esophagus (food pipe). F...

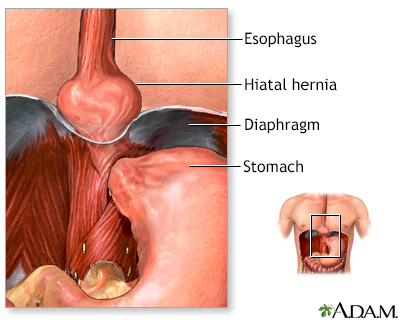
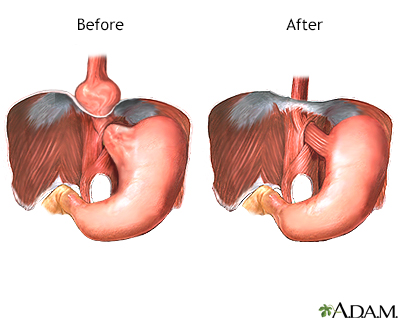
Reflux often occurs if the muscles where the esophagus meets the stomach do not close tightly enough. A hiatal hernia can make GERD symptoms worse. It occurs when the stomach bulges through this opening into your chest.
Hiatal hernia
Hiatal hernia is a condition in which part of the stomach extends through an opening of the diaphragm into the chest. The diaphragm is the sheet of ...

Symptoms of reflux or heartburn are burning in the stomach that you may also feel in your throat or chest, burping or gas bubbles, or trouble swallowing food or fluids.
Description
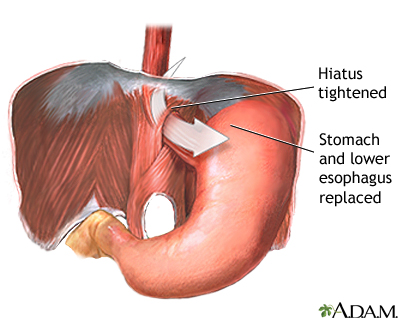
The most common procedure of this type is called fundoplication. In this surgery, your surgeon will:
- First repair the hiatal hernia, if one is present. This involves tightening the opening in your diaphragm with stitches to keep your stomach from bulging upward through the opening in the muscle wall. Some surgeons place a piece of mesh in the repaired area to make it more secure.
- Wrap the upper part of your stomach around the end of your esophagus with stitches. The stitches create pressure at the end of your esophagus, which helps prevent stomach acid and food from flowing up from the stomach into the esophagus.
Surgery is done while you are under general anesthesia, so you are asleep and pain-free. Surgery most often takes 2 to 3 hours. Your surgeon may choose from different techniques.
OPEN REPAIR
- Your surgeon will make 1 large surgical cut in your belly.
- A tube may be inserted into your stomach through the abdomen to keep the stomach wall in place. This tube will be taken out in about a week.
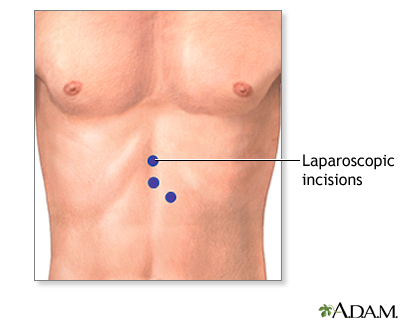
LAPAROSCOPIC REPAIR
- Your surgeon will make 3 to 5 small cuts in your belly. A thin tube with a tiny camera on the end is inserted through one of these cuts.
- Surgical tools are inserted through the other cuts. The laparoscope is connected to a video monitor in the operating room.
- Your surgeon does the repair while viewing the inside of your belly on the monitor.
- Your surgeon may need to switch to an open procedure in case of problems.
ENDOLUMINAL FUNDOPLICATION
- This is a new procedure that can be done without making cuts. A special camera on a flexible tool (endoscope) is passed down through your mouth and into your esophagus.
- Using this tool, the surgeon will put small clips in place at the point where the esophagus meets the stomach. These clips help prevent food or stomach acid from backing up.
Why the Procedure Is Performed
Before surgery is considered, your health care provider will have you try:
- Medicines such as H2 blockers or PPIs (proton pump inhibitors)
H2 blockers
H2 blockers are medicines that work by reducing the amount of stomach acid secreted by glands in the lining of your stomach.
Read Article Now Book Mark ArticlePPIs
Proton pump inhibitors (PPIs) are medicines that work by reducing the amount of stomach acid made by glands in the lining of your stomach.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Lifestyle changes
Lifestyle changes
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents leak backwards from the stomach into the esophagus (the tube from...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Surgery to treat your heartburn or reflux symptoms may be recommended when:
- Your symptoms do not get much better when you use medicines.
- You do not want to keep taking these medicines.
- You have more severe problems in your esophagus, such as scarring or narrowing, ulcers, or bleeding.
- You have reflux disease that is causing aspiration pneumonia, a chronic cough, or hoarseness.
Anti-reflux surgery is also used to treat a problem where part of your stomach is getting stuck in your chest or is twisted. This is called a para-esophageal hernia.
Risks
Risks of any anesthesia and surgery in general are:
- Reactions to medicines
-
Breathing problems
Breathing problems
Breathing difficulty may involve:Difficult breathing Uncomfortable breathingFeeling like you are not getting enough air
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Bleeding, blood clots, or infections
Bleeding
Bleeding is the loss of blood. Bleeding may be:Inside the body (internal)Outside the body (external)Bleeding may occur:Inside the body when blood le...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Risks of this surgery are:
- Damage to the stomach, esophagus, liver, or small intestine. This is very rare.
- Gas bloat. This is when the stomach overfills with air or food and you are unable to relieve the pressure by burping or vomiting. These symptoms slowly get better for most people.
- Pain and difficulty when you swallow. This is called dysphagia. In most people, this goes away during the first 3 months after surgery.
- Return of the hiatal hernia or reflux.
Before the Procedure
You may need the following tests:
- Blood tests (complete blood count, electrolytes, or liver tests).
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleElectrolytes
Electrolytes are minerals in your blood and other body fluids that carry an electric charge. Electrolytes affect how your body functions in many ways...
Read Article Now Book Mark Article - Esophageal manometry (to measure pressures in the esophagus) or pH monitoring (to see how much stomach acid is coming back into your esophagus).
PH monitoring
Esophageal pH monitoring is a test that measures how often stomach acid enters the tube that leads from the mouth to the stomach (called the esophagu...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Upper endoscopy. Almost all people who have this anti-reflux surgery have already had this test. If you have not had this test, you will need to have it.
- X-rays of the esophagus.
Always tell your provider if:
- You could be pregnant.
- You are taking any medicines, or supplements or herbs you bought without a prescription.
Before your surgery:
- You may need to stop taking aspirin, ibuprofen (Advil, Motrin), vitamin E, clopidogrel (Plavix), warfarin (Coumadin), and any other medicines or supplements that affect blood clotting several days before surgery. Ask your surgeon what you should do.
- Ask your provider which medicines you should still take on the day of your surgery.
On the day of your surgery:
- Follow your surgeon's instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Follow instructions for showering before surgery.
Your surgeon will tell you when to arrive at the hospital. Be sure to arrive on time.
After the Procedure
Most people who have laparoscopic surgery can leave the hospital within 1 to 3 days after the procedure. You may need a hospital stay of 2 to 6 days if you have open surgery. Most people can return to normal activities in 4 to 6 weeks.
Leave the hospital
You had surgery to treat your gastroesophageal reflux disease (GERD). GERD is a condition that causes food or liquid to come up from your stomach in...
Outlook (Prognosis)
Heartburn and other symptoms should improve after surgery. Some people still need to take medicines for heartburn after surgery.
You may need another surgery in the future if you develop new reflux symptoms or swallowing problems. This may happen if your stomach was wrapped around your esophagus too tightly, the wrap loosens, or a new hiatal hernia develops.
References
Jhu J, Oelschlager BK. Esophagus: surgical management of gastroesophageal reflux disease. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:3-80.
Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022 ;117(1):27-56. PMID: 34807007 pubmed.ncbi.nlm.nih.gov/34807007/.
Richter JE, Vaezi MF. Gastroesophageal reflux disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 46.
Yates RB, Oelschlager BK, Pellegrini CA. Gastroesophageal reflux disease and hiatal hernia. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 43.
-
Hiatal hernia repair - series
Presentation
-
Hiatal hernia - X-ray - illustration
This X-ray shows the upper portion of the stomach protruding through the diaphragm (hiatal hernia).
Hiatal hernia - X-ray
illustration
Review Date: 11/25/2023
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.