Large bowel resection
Ascending colectomy; Descending colectomy; Transverse colectomy; Right hemicolectomy; Left hemicolectomy; Low anterior resection; Sigmoid colectomy; Subtotal colectomy; Proctocolectomy; Colon resection; Laparoscopic colectomy; Colectomy - partial; Abdominal perineal resectionLarge bowel resection is surgery to remove all or part of your large bowel. This surgery is also called colectomy. The large bowel is also called the large intestine or colon.
- Removal of the entire colon and the rectum is called a proctocolectomy.
- Removal of all of the colon but not the rectum is called subtotal colectomy.
- Removal of part of the colon but not the rectum is called a partial colectomy.
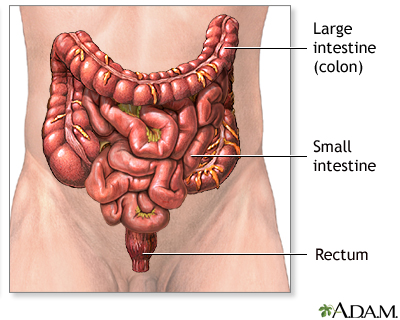
The large bowel connects the small intestine to the anus. Normally, stool passes through the large bowel before leaving the body through the anus.
Description
You'll receive general anesthesia at the time of your surgery. This will keep you asleep and pain-free.
General anesthesia
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
The surgery can be performed laparoscopically, with open surgery, or robotically. Depending on which surgery you have, the surgeon will make one or more cuts (incisions) in your belly.
If you have laparoscopic or robotic surgery:
- The surgeon makes 3 to 5 small cuts (incisions) in your belly. A medical device called a laparoscope is inserted through one of the cuts. The scope is a thin, lighted tube with a camera on the end. It lets the surgeon see inside your belly. Other medical instruments are inserted through the other cuts.
- A cut of about 2 to 3 inches (in) or 5 to 7.6 centimeters (cm) may also be made if your surgeon needs to put their hand inside your belly to feel or remove the diseased bowel.
- Your belly is filled with a harmless gas to expand it. This makes the area easier for the surgeon to see and work in.
- Your surgeon examines the organs in your belly to see if there are any problems.
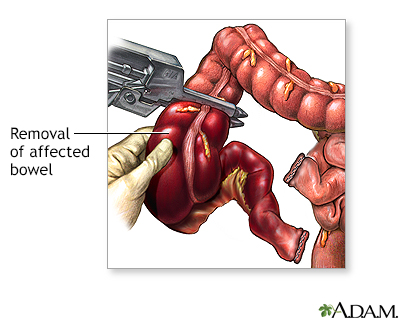
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
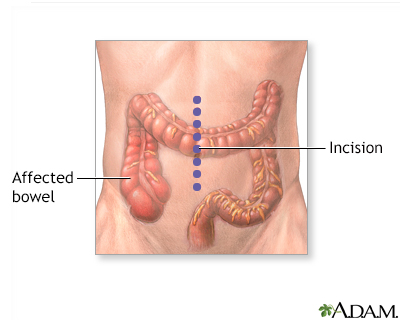
If you have open surgery:
- Your surgeon makes a cut of 6 to 8 in (15.2 to 20.3 cm) in your lower belly.
- The organs in your belly are examined to see if there are any problems.
- The diseased part of your large bowel is located and removed. Some lymph nodes may also be removed.
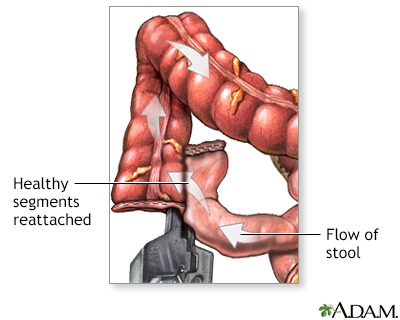
In both kinds of surgery, the next steps are:
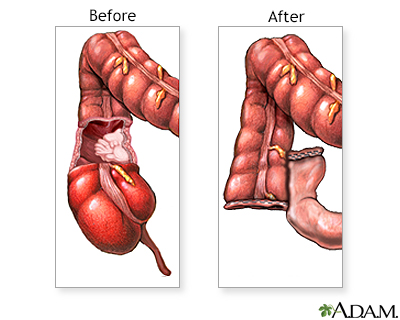
- If there is enough healthy large intestine left, the ends are stitched or stapled together. This is called an anastomosis. Most people have this step done.
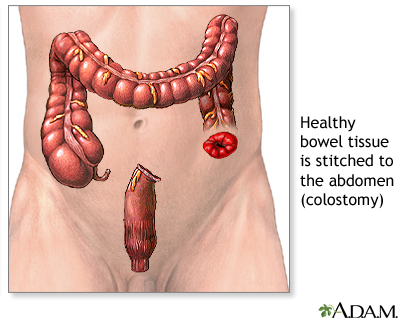
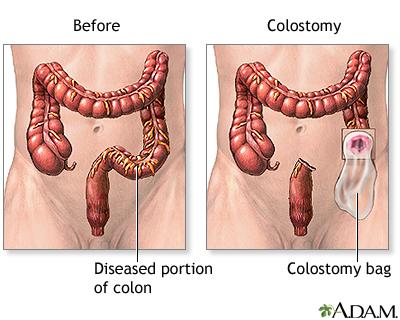
- If there is not enough healthy large intestine to reconnect, the surgeon makes an opening called a stoma through the skin of your belly. The colon is attached to the outer wall of your belly. Stool will go through the stoma into a drainage bag outside your body. This is called a colostomy. The colostomy may be either short-term or permanent. If the colostomy is short term, another surgical procedure will be needed later to reconnect the bowel and close the colostomy site.
Colostomy
Colostomy is a surgical procedure that brings one end of the large intestine out through an opening (stoma) made in the abdominal wall. Stools movin...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Colectomy usually takes between 1 and 4 hours.
Why the Procedure Is Performed
Large bowel resection is used to treat many conditions, including:
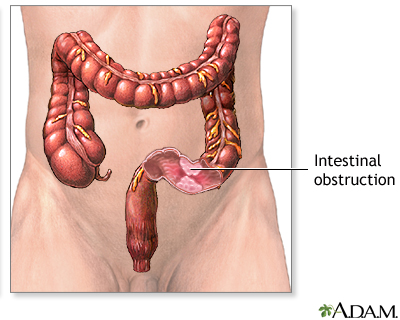
-
A blockage in the intestine due to scar tissue
A blockage in the intestine
Intestinal obstruction is a partial or complete blockage of the bowel. The contents of the intestine cannot pass through it.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Colon cancer
Colon cancer
Colorectal cancer is cancer that starts in the large intestine (colon) or the rectum (end of the colon). It is also sometimes simply called colon ca...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Diverticular disease (disease of the large bowel)
Diverticular disease
Diverticula are small, bulging sacs or pouches that form on the inner wall of the intestine. Diverticulitis occurs when these pouches become inflame...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Other reasons for bowel resection are:
-
Familial polyposis (polyps are growths on the lining of the colon or rectum)
Familial polyposis
A colorectal polyp is a growth on the lining of the colon or rectum.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Injuries that damage the large bowel
- Intussusception (when one part of the intestine pushes into another)
- Precancerous polyps
- Twisting of the bowel (volvulus)
-
Ulcerative colitis
Ulcerative colitis
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Severe bleeding from the large intestine
- Lack of nerve function to the large intestine
Risks
Risks for anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Infection, including the lungs or bladder
- Nausea and vomiting
Risks for this surgery are:
- Bleeding inside your belly
- Bulging tissue through the surgical cut, called an incisional hernia
Hernia
A groin lump is swelling in the groin area. This is where the upper leg meets the lower abdomen.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Damage to nearby organs in the body
- Damage to the ureter or bladder
- Problems with the colostomy
- Scar tissue that forms in the belly and causes a blockage of the intestines
- The edges of your intestines that are sewn together come open (anastomotic leak, which may be life threatening)
- Wound breaking open
- Wound infection
-
Peritonitis
Peritonitis
Peritonitis is an inflammation (irritation) of the peritoneum. This is the thin tissue that lines the inner wall of the abdomen and covers most of t...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Before the Procedure
Talk with your surgeon or nurse about how surgery will affect:
- Intimacy and sexuality
- Pregnancy
- Sports
- Work
Tell your surgeon or nurse if:
- You are or could be pregnant.
- You are taking any medicines, including medicines, drugs, supplements, or herbs you bought without a prescription.
- You have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
Planning for your surgery:
- If you have diabetes, heart disease, or other medical conditions, your surgeon may ask you to see the health care provider who treats you for these conditions.
Diabetes
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHeart disease
Coronary heart disease is a narrowing of the blood vessels that supply blood and oxygen to the heart. Coronary heart disease (CHD) is also called co...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
If you smoke, it's important to cut back or quit. Smoking can slow healing and increase the risk for blood clots. Ask your provider for help quitting smoking.
If you smoke, it's important to cut bac...
There are many ways to quit smoking. There are also resources to help you. Family members, friends, and co-workers may be supportive. But to be su...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleBlood clots
Blood clots are clumps that occur when blood hardens from a liquid to a solid. A blood clot that forms inside one of your veins or arteries is calle...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - If needed, prepare your home to make it easier to recover after surgery.
Prepare your home
Getting your home ready after you have been in the hospital often requires some preparation. Set up your home to make your life easier and safer when...
Read Article Now Book Mark Article - Ask your surgeon if you need to arrange to have someone drive you home after your surgery.
- You may be asked to go through a bowel preparation to clean your intestines of all stool. This may involve staying on a liquid diet for a few days and using laxatives.
During the weeks before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
- Let your surgeon know about any illness you may have before your surgery. This includes COVID-19, cold, flu, fever, herpes breakout, or other illness. If you do get sick, your surgery may need to be postponed.
COVID-19
Coronavirus disease 2019 (COVID-19) is a respiratory illness that causes fever, coughing, and shortness of breath, but many other symptoms can occur....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCold
The common cold most often causes a runny nose, nasal congestion, and sneezing. You may also have a sore throat, cough, headache, or other symptoms....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFlu
The flu (influenza) is a viral respiratory illness that causes fever, chills, runny nose, body aches, and cough. It spreads easily from person to pe...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleFever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You may be asked to drink only clear liquids such as broth, clear juice, and water on the day before surgery.
After the Procedure
You will be in the hospital for 3 to 7 days. You may have to stay longer if the colectomy was an emergency operation.
You may also need to stay longer if a large amount of your large intestine was removed or if you develop problems after the surgery.
By the second or third day, you will probably be able to drink clear liquids. Thicker fluids and then soft foods will be added as your bowel begins to work again.
After you go home, follow instructions on how to take care of yourself as you heal.
Follow instructions
You had surgery to remove all or part of your large intestine (large bowel). You may also have had a colostomy. This article describes what to expe...
Outlook (Prognosis)
Most people who have a large bowel resection recover fully. Even with a colostomy, most people are able to do the activities they were doing before their surgery. This includes most sports, travel, gardening, hiking, other outdoor activities, and most types of work.
If you have a long-term (chronic) condition, such as cancer, Crohn disease, or ulcerative colitis, you may need ongoing medical treatment.
Crohn disease
Crohn disease is a disease where parts of the digestive tract become inflamed. It most often involves the lower end of the small intestine and the be...

Ulcerative colitis
Ulcerative colitis is a condition in which the lining of the large intestine (colon) and rectum become inflamed. It is a form of inflammatory bowel ...

References
Albers BJ, Lamon DJ. Colon repair/colostomy creation. In: Baggish MS, Karram MM, eds. Atlas of Pelvic Anatomy and Gynecologic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 96.
Galandiuk S, Netz U, Morpurgo E, Tosato SM, Abu-Freha N, Ellis CT. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 52.
-
The large intestine - illustration
The large intestine (or colon, or large bowel) is the last structure to process food, taking the undigestible matter from the small intestine, absorbing water from it and leaving the waste product called feces. Feces are expelled from the body through the rectum and the anus.
The large intestine
illustration
-
Colostomy - Series
Presentation
-
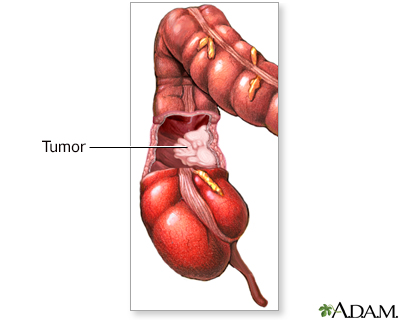
Large bowel resection - Series
Presentation
-
Blood supply of the large intestine - illustration
The blood supply to the large intestine originates in the superior and inferior mesenteric arteries.
Blood supply of the large intestine
illustration
-
The large intestine - illustration
The large intestine (or colon, or large bowel) is the last structure to process food, taking the undigestible matter from the small intestine, absorbing water from it and leaving the waste product called feces. Feces are expelled from the body through the rectum and the anus.
The large intestine
illustration
-
Colostomy - Series
Presentation
-
Large bowel resection - Series
Presentation
-
Blood supply of the large intestine - illustration
The blood supply to the large intestine originates in the superior and inferior mesenteric arteries.
Blood supply of the large intestine
illustration
Review Date: 1/21/2025
Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.



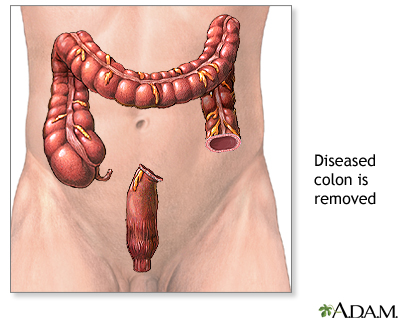

![<strong>Large bowel resection - series</strong><p>The large bowel [large intestine or the colon] is part of the digestive system. It runs from the small intestine to the rectum. It is made up of three portions; the ascending, transverse and descending colon. The ascending colon is sometimes referred to as the right colon; the descending colon is sometimes referred to as the left, or sigmoid colon.</p>](../../graphics/images/en/10255.jpg)