Knee joint replacement
Total knee replacement; Knee arthroplasty; Knee replacement - total; Tricompartmental knee replacement; Subvastus knee replacement; Knee replacement - minimally invasive; Knee arthroplasty - minimally invasive; TKA - knee replacement; Osteoarthritis - replacement; OA - knee replacementKnee joint replacement is a surgery to replace a knee joint with a man-made artificial joint. The artificial joint is called a prosthesis.
Prosthesis
A prosthesis is a device designed to replace a missing part of the body or to make a part of the body work better. Diseased or missing eyes, arms, h...

Description
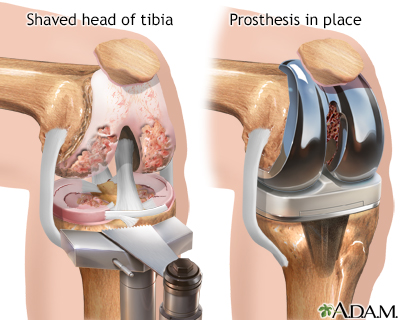
Damaged cartilage and bone are removed from the knee joint. Man-made pieces are then placed in the knee.
These pieces may be placed in the following places in the knee joint:
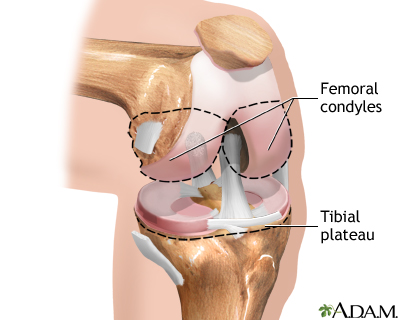
- Lower end of the thigh bone -- This bone is called the femur. The replacement part is usually made of metal.
- Upper end of the shin bone, which is the large bone in your lower leg -- This bone is called the tibia. The replacement part is usually made from metal and strong plastic.
- Back side of your kneecap -- Your kneecap is called the patella. The replacement part is usually made from a strong plastic.
You will not feel any pain during the surgery. You will have one of these two types of anesthesia:
-
General anesthesia -- This means you will be asleep and unable to feel pain.
General anesthesia --
General anesthesia is treatment with certain medicines that puts you into a deep sleep-like state so you do not feel pain during surgery. After you ...
Read Article Now Book Mark Article - Regional (spinal or epidural) anesthesia -- Medicine is put into your spine to make you numb below your waist. You will also get medicine to make you sleepy. And you may get medicine that will make you forget about the procedure, even though you are not fully asleep.
Spinal or epidural
Spinal and epidural anesthesia are procedures that deliver medicines that numb parts of your body to block pain. They are given through shots in or ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
After you receive anesthesia, your surgeon will make a cut over your knee to open it up. This cut is often 8 to 10 inches (20 to 25 centimeters) long. Then your surgeon will:
- Move your kneecap out of the way
- Cut the ends of your thigh bone and shin (lower leg) bone to fit the replacement part.
- Cut the underside of your kneecap to prepare it for the new pieces that will be attached there.
- Fasten the two parts of the prosthesis to your bones. One part will be attached to the end of your thigh bone and the other part will be attached to your shin bone. The pieces can be attached using bone cement or screws.
- Attach the underside of your kneecap. A special bone cement is used to attach this part.
- Repair (if needed) your muscles and tendons around the new joint and close the surgical cut.
The surgery takes about 2 hours.
Most artificial knees have both metal and plastic parts. Some surgeons now use different materials, including metal on metal, ceramic on ceramic, or ceramic on plastic.
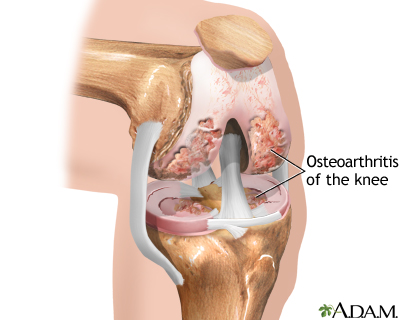
Why the Procedure Is Performed
The most common reason to have a knee joint replaced is to relieve severe arthritis pain. Your health care provider may recommend knee joint replacement if:
- You are having pain from knee arthritis that keeps you from sleeping or doing normal activities.
- You cannot walk and take care of yourself.
- Your knee pain has not improved with other treatment.
- You understand what surgery and recovery will be like.
Most of the time, knee joint replacement is done in people age 60 and older. Younger people who have a knee joint replaced may put extra stress on the artificial knee and cause it to wear out early and not last as long.
Before the Procedure
Always tell your provider what medicines you are taking, even medicines, supplements, or herbs you bought without a prescription.
During the 2 weeks before your surgery:
-
Prepare your home for when you leave the hospital.
Prepare your home
Before you go to the hospital for surgery, set up your home to make your recovery and life easier when you come back. Plan and do this well in advan...
Read Article Now Book Mark Article - One to two weeks before surgery, you may be asked to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), blood thinners such as warfarin (Coumadin), or clopidogrel (Plavix), and other medicines (such as Eliquis or Xarelto).
- You may also need to stop taking medicines that can make your body more likely to get an infection. These include methotrexate, etanercept (Enbrel), or other medicines that suppress your immune system. Make sure you ask your providers when it is safe to resume taking these medicines.
- Ask your surgeon which medicines you should still take on the day of your surgery.
- If you have diabetes, heart disease, or other medical conditions, your surgeon may ask you to see the provider who treats you for these conditions to see if it is safe for you to have the surgery.
- Tell your provider and surgeon if you have been drinking a lot of alcohol, more than 1 or 2 drinks per day.
- If you smoke, you need to stop. Ask your providers for help. Smoking will slow down wound and bone healing. Your recovery may not be as good if you keep smoking.
- Always let your surgeon know about any cold, flu, fever, herpes breakout, or other illness you have before your surgery.
Fever
Fever is the temporary increase in the body's temperature in response to a disease or illness. A child has a fever when the temperature is at or abov...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleHerpes
Herpes viral culture of a lesion is a lab test to check if a skin sore is infected with the herpes virus.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - You may want to visit a physical therapist to learn some exercises to do before surgery.
- Practice using a cane, walker, crutches, or a wheelchair correctly.
Walker
It is important to start walking soon after a leg injury or surgery. But you will need support while your leg is healing. A walker can give you sup...
Read Article Now Book Mark ArticleCrutches
It is important to start walking as soon as you can after your surgery. But you will need support for walking while your leg heals. Crutches may be...
Read Article Now Book Mark Article
On the day of your surgery:
- You will most often be asked not to drink or eat anything for 6 to 12 hours before the procedure.
- Take the medicines you have been told to take with a small sip of water.
- You will be told when to arrive at the hospital.
After the Procedure
You may go home the same day or you may stay in the hospital for 1 to 2 days. During that time, you will recover from your anesthesia and from the surgery itself. You will be asked to start moving and walking as soon as the day of surgery.
Hospital for 1 to 2 days
Most often, you will stay in the hospital for 1 to 2 days after having hip or knee joint replacement surgery. During that time, you will recover fro...
Full recovery will take 4 months to a year.
Some people need a short stay in a rehabilitation center after they leave the hospital and before they go home. At a rehabilitation center, you will learn how to safely do your daily activities on your own.
Outlook (Prognosis)
The results of a total knee replacement are often excellent. The operation relieves pain for most people. Most people do not need help walking after they fully recover.
Over 90 percent of artificial knee joints last over 15 years. Some last as long as 25 years before they loosen and need to be replaced again. Total knee replacements can be replaced again if they get loose or wear out. However, in most cases the results are not as good as the first time. It is important not to have the surgery too early so you will need another surgery at a young age or have it too late when you will not benefit the most. After surgery, you should have periodic checkups with your surgeon to make sure the parts of your artificial joint are in good position and condition.
References
American Academy of Orthopedic Surgeons (AAOS) website. Treatment: total knee replacement. orthoinfo.aaos.org/en/treatment/total-knee-replacement. Updated February 2024. Accessed September 26, 2024.
Ellen MI, Forbush DR, Groomes TE. Total knee arthroplasty. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 80.
Mihalko WM. Arthroplasty of the knee. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics.14th ed. Philadelphia, PA: Elsevier; 2021:chap 7.
-
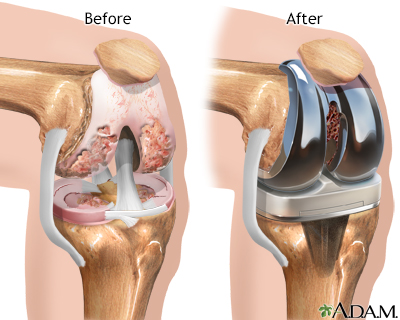
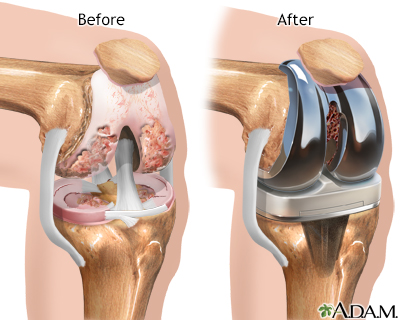
Knee joint replacement prosthesis - illustration
A prosthesis is a device designed to replace a missing part of the body, or to make a part of the body work better. The metal prosthetic device in knee joint replacement surgery replaces cartilage and bone which is damaged from disease or aging.
Knee joint replacement prosthesis
illustration
-
Knee joint replacement - Series
Presentation
-
Knee joint replacement prosthesis - illustration
A prosthesis is a device designed to replace a missing part of the body, or to make a part of the body work better. The metal prosthetic device in knee joint replacement surgery replaces cartilage and bone which is damaged from disease or aging.
Knee joint replacement prosthesis
illustration
-
Knee joint replacement - Series
Presentation
Review Date: 8/27/2024
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.