Helicobacter pylori infection
H pylori infection
Helicobacter pylori (H pylori) is a type of bacteria that infects the stomach. It is very common, affecting about two thirds of the world's population. H pylori infection is the most common cause of peptic ulcers. However, the infection does not cause problems for most people.
Peptic ulcers
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric ulcer) or in the first part of the small intestine (duodenal ulcer)....

Causes
H pylori bacteria are most likely passed directly from person to person. This tends to happen during childhood. The infection remains throughout life if not treated.
It's not clear how the bacteria are passed from one person to another. The bacteria may spread from:
- Mouth-to-mouth contact
- GI tract illness (particularly when vomiting occurs)
- Contact with stool (fecal material)
- Contaminated food and water
The bacteria may trigger ulcers in the following way:
- H pylori enters the mucus layer of the stomach and attaches to the stomach lining.
- H pylori cause the stomach to produce more stomach acid. This damages the stomach lining, leading to ulcers in some people.
Besides ulcers, H pylori bacteria can also cause a chronic inflammation in the stomach (gastritis) or the upper part of the small intestine (duodenitis) and duodenal ulcers.
Chronic
Chronic refers to something that continues over an extended period of time. A chronic condition is usually long-lasting and does not easily or quick...

H pylori can also sometimes lead to stomach cancer or a rare type of stomach lymphoma.
Symptoms
About 10% to 15% of people infected with H pylori develop peptic ulcer disease. Small ulcers may not cause any symptoms. Some ulcers can cause serious bleeding.
An aching or burning pain in your abdomen is a common symptom. The pain may be worse with an empty stomach. The pain can differ from person to person, and some people have no pain.
Other symptoms include:
- Feeling of fullness or bloating and problems drinking as much fluid as usual
- Hunger and an empty feeling in the stomach, often 1 to 3 hours after a meal
- Mild nausea that may go away with vomiting
- Loss of appetite
- Weight loss without trying
- Burping
-
Bloody or dark, tarry stools or bloody vomit
Bloody or dark, tarry stools
Black or tarry stools with a foul smell are a sign of a problem in the upper digestive tract. It most often indicates that there is bleeding in the ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider may test you for H pylori if you:
- Have peptic ulcers or a history of ulcers
- Have discomfort and pain in the stomach lasting more than a month
Tell your provider about the medicines you take. Nonsteroidal anti-inflammatory drugs (NSAIDs) can also cause ulcers. If you have an ulcer or show symptoms of an H pylori infection, your provider may perform the following tests for H pylori
H pylori
Helicobacter pylori (H pylori) is the bacteria (germ) responsible for most stomach (gastric) and duodenal ulcers and many cases of stomach inflammati...

- Breath test -- urea breath test (Carbon Isotope-urea Breath Test, or UBT). Your provider will ask you to swallow a special substance that has urea. If H pylori are present, the bacteria turn the urea into carbon dioxide. This is detected and recorded in your exhaled breath after 10 minutes.
- Blood test-- measures antibodies to H pylori in your blood.
- Stool test -- detects the presence of H pylori in your stool.
-
Biopsy -- tests a tissue sample taken from the stomach lining using endoscopy. The sample is checked for H pylori infection.
Biopsy
A biopsy is the removal of a small piece of tissue for lab examination.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleEndoscopy
Endoscopy is a way of looking inside the body using a flexible tube that has a small camera and light on the end of it. This instrument is called an...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
In order for your ulcer to heal and to reduce the chance it will come back, you will be given medicines to:
- Kill the H pylori bacteria (if present)
- Reduce acid levels in your stomach
Take all of your medicines as you have been told. Other lifestyle changes can also help.
Lifestyle changes
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric ulcer) or upper part of the small intestine (duodenal ulcer). This ...

If you have a peptic ulcer and an H pylori infection, treatment is recommended. The standard treatment involves different combinations of the following medicines for 10 to 14 days:
- Antibiotics to kill H pylori
- Proton pump inhibitors to help lower acid levels in the stomach
- Bismuth (the main ingredient in Pepto-Bismol) may be added to help kill the bacteria
Taking all of these medicines for up to 14 days is not easy. But doing so gives you the best chance for getting rid of the H pylori bacteria and preventing ulcers in the future.
Outlook (Prognosis)
If you take your medicines, there is a good chance that the H pylori infection will be cured. You will be much less likely to get another ulcer.
Sometimes, H pylori can be hard to fully cure. Repeated courses of different treatments may be needed. A stomach biopsy will sometimes be done to test the germ to see which antibiotic might work best. This can help guide future treatment. In some cases, H pylori can't be cured with any therapy, though the symptoms may be reduced.
If cured, reinfection may occur in areas where sanitary conditions are poor.
Posssible Complications
A chronic infection with H pylori may lead to:
-
Peptic ulcer disease
Peptic ulcer
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric ulcer) or in the first part of the small intestine (duodenal ulcer)....
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Chronic inflammation
- Gastric and upper intestine ulcers
-
Stomach cancer
Stomach cancer
Stomach cancer is cancer that starts in the stomach.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Gastric mucosa-associated lymphoid tissue (MALT) lymphoma
Other complications may include:
- Severe blood loss
- Scarring from an ulcer may make it harder for the stomach to empty
- Perforation or hole of the stomach and intestines
- Iron deficiency anemia
When to Contact a Medical Professional
Severe symptoms that begin suddenly may indicate a blockage in the intestine, perforation, or hemorrhage, all of which are emergencies. Symptoms may include:
- Tarry, black, or bloody stools
- Severe vomiting, which may include blood or a substance with the appearance of coffee grounds (a sign of a serious hemorrhage) or the entire stomach contents (a sign of intestinal obstruction)
- Severe abdominal pain, with or without vomiting or evidence of blood
Anyone who has any of these symptoms should go to the emergency room right away.
References
Chan FKL, Lau JYW. Peptic ulcer disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 53.
Cover TL, Blaser MJ. Helicobacter pylori and other gastric Helicobacter species. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 217.
Ku GY, Ilson DH. Cancer of the stomach. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 72.
-
Stomach - illustration
The stomach is the portion of the digestive system most responsible for breaking down food. The lower esophageal sphincter at the top of the stomach regulates food passing from the esophagus into the stomach, and prevents the contents of the stomach from reentering the esophagus. The pyloric sphincter at the bottom of the stomach governs the passage of food out of the stomach into the small intestine.
Stomach
illustration
-
Esophagogastroduodenoscopy (EGD) - illustration
Esophagogastroduodenoscopy (EGD) is a test procedure to examine the lining of the esophagus, stomach, and first part of the small intestine. The procedure uses an endoscope. This is a flexible tube with a light and camera at the end. A biopsy can be taken through the endoscope of any suspicious areas that are seen.
Esophagogastroduodenoscopy (EGD)
illustration
-
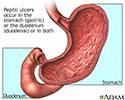
Location of peptic ulcers - illustration
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric) or the upper part of the small intestine (duodenal).
Location of peptic ulcers
illustration
-
Stomach - illustration
The stomach is the portion of the digestive system most responsible for breaking down food. The lower esophageal sphincter at the top of the stomach regulates food passing from the esophagus into the stomach, and prevents the contents of the stomach from reentering the esophagus. The pyloric sphincter at the bottom of the stomach governs the passage of food out of the stomach into the small intestine.
Stomach
illustration
-
Esophagogastroduodenoscopy (EGD) - illustration
Esophagogastroduodenoscopy (EGD) is a test procedure to examine the lining of the esophagus, stomach, and first part of the small intestine. The procedure uses an endoscope. This is a flexible tube with a light and camera at the end. A biopsy can be taken through the endoscope of any suspicious areas that are seen.
Esophagogastroduodenoscopy (EGD)
illustration
-
Location of peptic ulcers - illustration
A peptic ulcer is an open sore or raw area in the lining of the stomach (gastric) or the upper part of the small intestine (duodenal).
Location of peptic ulcers
illustration
Review Date: 3/31/2024
Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.